-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammad Arammash, Hosam Arammash, Shareef Syed, Use of ICG dye for urinary tract identification during robotic peritoneal window creation for a post-kidney transplant lymphocele, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae515, https://doi.org/10.1093/jscr/rjae515
Close - Share Icon Share
Abstract
Minimally invasive surgical creation of a peritoneal window for the treatment of lymphoceles post-kidney transplant is an effective procedure that comes with an elevated risk of iatrogenic injury to the urinary tract. Here, we present indocyanine green dye injection through a ureteral stent for intraoperative identification and avoidance of the transplant collecting system during peritoneal window creation. The procedure was successful and allowed for the resolution of the lymphocele without complication.
Introduction
The development of a lymphocele is a common complication following kidney transplantation that can result in graft dysfunction through the compression of the allograft or surrounding vasculature [1]. The incidence of symptomatic lymphoceles has been reported to be as high as 26% [2]. Synthetic polyethylene glycol sealant to ligate lymphatic vessels and the prophylactic fenestration of the peritoneum have been investigated as methods to prevent the development of a lymphocele [1, 3]. The creation of a peritoneal window through open surgery has previously been the preferred treatment for lymphoceles as it offers a lower rate of recurrence compared to percutaneous drainage and avoids the creation of dense scar tissue around the transplanted kidney caused by the injection of sclerosing substances such as povidone-iodine. However, open repair is associated with a risk of wound dehiscence, infection, ileus, patient discomfort, and changes in immunosuppression administration [4]. Creating a peritoneal window laparoscopically effectively treats lymphoceles and reduces recurrence risk. However, the approach has been shown to come with a 300% increased risk of iatrogenic lesions to the urinary tract compared with open repair [4, 5]. In a review of the literature and patients at their institution, Ancona et al. found that out of 252 patients, 129 had a lymphocele treated through open surgery while 123 were treated laparoscopically. Of those treated with open surgery, 1.6% suffered iatrogenic injury to the urinary tract compared to 7% in the laparoscopic group. However, the recurrence rate of lymphoceles was 15% in the open repair group compared to 4% in the laparoscopic group. The length of the laparoscopic operations ranged from 70 to 200 min, with a median of 120 min. While the lymphocele itself can be identified through the injection of methylene blue dye and the bladder can be identified through being filled with saline using a Foley catheter, there is a need for effective forms of identification of the ureter [4]. This report describes using indocyanine green (ICG) dye to visualize the transplant collecting system for the robotic creation of a peritoneal window.
Case report
The patient was a 53-year-old woman who presented with chronic kidney disease stage 4 attributed to hypertension. Preoperative BUN was 40, while creatinine was 3.78. The living donor kidney transplant was completed without initial complications. By the discharge date, the creatinine had down trended to 0.99 with a BUN of 20.
Approximately four weeks later, the patient presented for a kidney biopsy due to an elevated creatinine of 1.56 and BUN of 30 and was noted to have a right lateral perinephric collection measuring 165 mL on ultrasound. The biopsy was negative for rejection. Ultrasound-guided drainage of 140 mL of the peri-allograft collection in the right lower quadrant improved serum creatinine. The aspirated fluid was negative for bacterial and fungal growth. The fluid was 95% lymphocytes, confirming the diagnosis of a lymphocele. A planned follow-up ultrasound 4 days later revealed a re-accumulation of the right perinephric fluid collection measuring 5.4 × 8.5 × 7.2 cm3 (volume 173 mL), with minimal complexity. A new mild hydroureteronephrosis, which did not improve post void, was also noted. A CT scan (Fig. 1) reported a peri-allograft fluid collection measuring 8.5 × 5.3 × 9.2 cm3 with localized mass effect onto the upper pole of the transplanted kidney. The patient was scheduled for a robotic peritoneal window creation with urology assistance with retrograde ICG instillation for intraoperative localization.
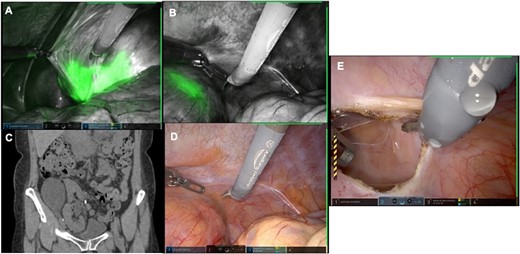
(A) Robotic Firefly visual display of the transplanted kidney inferior pole demonstrating ICG within the collecting system. (B) Robotic Firefly display of the transplant kidney superior pole demonstrating ICG within the parenchyma medial to the lymphocele. (C) CT scan with lateral position of lymphocele. (D) Conventional robotic display without ICG. (E) Completed peritoneal window with successful drainage of lymphocele.
Cystoscopy revealed a normal bladder and transplant ureter and anastomosis, without any lesions or erythema. The transplanted ureteral orifice was intubated with a 5 French stent over a wire. The retrograde pyelogram revealed a smooth contour of the renal pelvis and ureter with mild hydronephrosis in the right lower quadrant. The 5 French stent was advanced into the upper pole and 10 mL of ICG was instilled. The cystoscope was removed while keeping the stent in place.
A Veress needle was introduced at Palmer's point. The abdomen was insufflated to 15 mmHg. An 11-mm optical entry was used to enter the abdomen under direct visualization in the left flank. We performed a diagnostic laparoscopy. Two further 8-mm trocars and one 12-mm trocar were placed under direct vision in the left flank as working ports. The robot was docked.
On entry, firefly was able to identify the renal pelvis clearly (Fig. 1). Next, an area, overlying the lymphocele, clearly distal to the ICG was identified, and an opening into the lymphocele was created. There was significant drainage of golden fluid. A large defect was resected from the peritoneum and passed off the table. The robot was undocked. The total length of the procedure (cystoscopy and laparoscopy) was 69 min. There were no complications, and the estimated blood loss was minimal (5 mL).
Discussion
The patient tolerated the procedure well, and the post-op course was uneventful. Creatinine on discharge was 1.28, and BUN was 19. At a follow-up 6 weeks after the operation, ultrasound revealed no evidence of a recurrent lymphocele and a functional peritoneal window. The patient’s creatinine was stable at 1.23. The procedure was completed successfully without complications. Given the significantly increased risk of injury to the urinary tract seen with the laparoscopic creation of a peritoneal window, techniques for mitigating this risk are in demand. Lymphoceles are often positioned inferiorly and either anterior or posterior to the transplanted kidney and iliac vessels, necessitating the identification of the bladder, renal pelvis, and ureter before the creation of the peritoneal window to avoid iatrogenic injury. Injuries to the ureter are the most common, followed by the bladder and renal pelvis [4]. However, the ureter is the most difficult structure to identify. Though the available literature is sparse, the use of ICG dye for visualization of the urinary tract in robotic resection of bladder wall endometriosis has been described by Van Trappen et al. (2023) [6]. We successfully demonstrated using an ICG dye injection through a ureter stent to identify the transplant collecting system to prevent iatrogenic injury while creating a peritoneal window. The procedure was uncomplicated, reproducible, and fast while easily avoiding a significant potential complication that currently lacks adequate solutions.
Author contributions
Mohammad Arammash participated in writing of the paper. Hosam Arammash participated in writing of the paper. Shareef Syed performed procedure and participated in writing of the paper.
Conflict of interest statement
None declared.
Funding
None declared.



