-
PDF
- Split View
-
Views
-
Cite
Cite
Fidelis C Okoli, Sally Tan, Hazim Hakmi, Jacqueline Forman, Patrick A Hartendorp, An unusual case of giant jejunal diverticula presenting radiologically as toxic megacolon, Journal of Surgical Case Reports, Volume 2024, Issue 7, July 2024, rjae436, https://doi.org/10.1093/jscr/rjae436
Close - Share Icon Share
Abstract
Jejunal diverticulosis is an uncommon entity of the gastrointestinal tract. It involves the presence of multiple diverticula (pouches) in the jejunal wall. Jejunal diverticulosis is not so common, and the epidemiology is ill defined, but usually, it is known to affect the elderly more. They are considered from a pathophysiological point of view as motility disorders, structural defects, or high intraluminal pressures, with the result of prolapse of the mucosa of the jejunum through weak points of the intestinal wall. It represents a rare entity with different clinical presentations, ranging from being asymptomatic to life-threatening complications such as obstruction, bleeding, or perforation. Treatment depends on the presentation and can be conservative or surgical management.
Introduction
Jejunal diverticulosis is an uncommon pathology of the gastrointestinal tract with an incidence of 0.3%–2.3% [1]. It is defined by the presence of multiple diverticula (outpouchings) in the jejunal wall. Jejunal diverticula can be due to motility disorders, congenital structural defects, or high intraluminal pressures, resulting in prolapse of the jejunal mucosa through weak points at the intestinal wall [2]. Most patients remain asymptomatic, but some may present with abdominal pain due to acute complications such as obstruction, bleeding, perforation, and inflammation [3]. Herein, we present an unusual case of a massive jejunal diverticulum masquerading radiologically as toxic megacolon in a young adult female.
Case report
Eighteen-year-old female with a history of chronic constipation and a family history of inflammatory bowel disease presented to the emergency room with 2 days of hematochezia associated with lower abdominal pain. She was previously seen in the gastroenterology outpatient clinic and workup revealed normal fecal calprotectin and inflammatory markers. She had no prior endoscopic work up.
In the emergency department, she was afebrile, hypotensive, and tachycardic. Laboratory investigation was significant for leukocytosis with bandemia, hypokalemia, hyponatremia, and an elevated C-reactive protein of 229 mg/L. Computerized tomography of the abdomen and pelvis with intravenous contrast revealed dilated bowel with pneumatosis that was concerning for toxic megacolon (Fig. 1A and B).
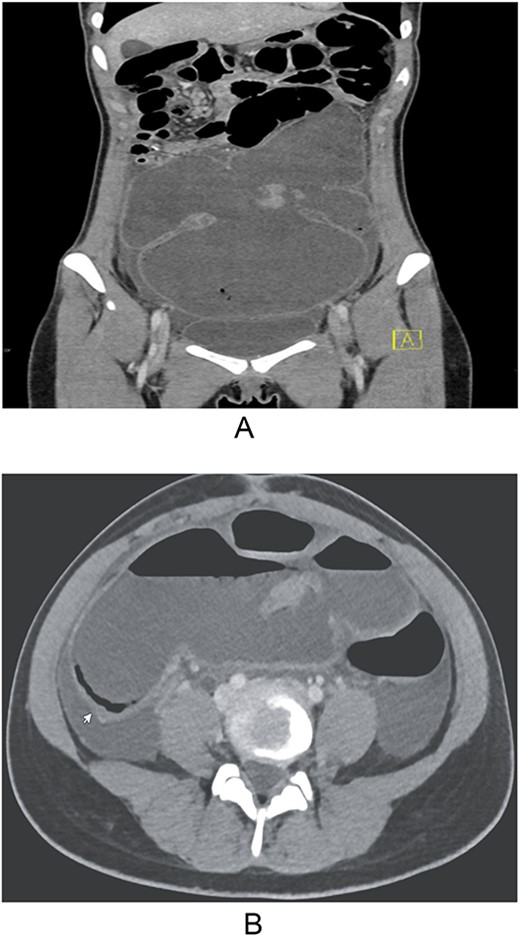
(A and B) Computerized tomography of the abdomen and pelvis with intravenous contrast showing dilated bowel with pneumatosis mimicking toxic megacolon.
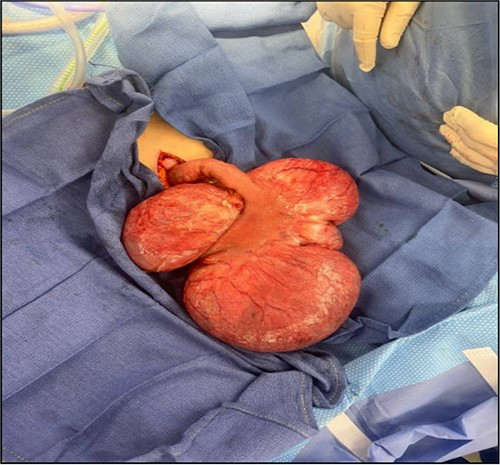
With concern for impending perforation and bowel ischemia, the patient was taken emergently for an exploratory laparotomy. Rigid proctoscopy revealed non-dilated rectum and sigmoid colon with healthy mucosa. Celiotomy was performed via vertical midline incision. A 25 cm × 25 cm mass contiguous to the distal jejunum with four saccular outpouchings was found occupying the pelvis (Fig. 2). The colon appeared non-dilated and viable. Segmental jejunal resection was performed to healthy margins, with primary side to side stapled anastomosis.
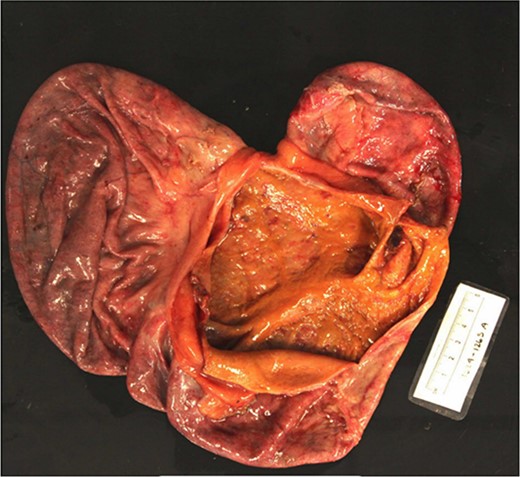
The patient’s postoperative course was uneventful. Gross tissue examination revealed transmural necrosis, acute serositis, and viable resection margins (Fig. 3). The outpouchings were found to include all layers of the intestinal wall signifying a true massive diverticulum with multiple compartments.
Discussion
The pathogenesis of jejunal diverticula is a multifactorial disease process. It is postulated that smooth muscle or myenteric plexus dysfunction arising from the peripheral nervous system leads to dysmotility. This dysmotility creates regions of raised intraluminal pressure that permit outpouching of mucosa through weak points in the bowel wall where blood vessels traverse the muscular layers. Chronic constipation is a significant risk factor as was present in our patient. Moreover, it is mostly commonly found in geriatric patients, signifying some form of degenerative change probably related to the changes in the intestinal wall's structure with age [4].
Jejunal diverticulosis can present as a variety of clinical manifestations. While most people will remain asymptomatic, others can become symptomatic, ranging from mild non-specific abdominal symptoms to devastating acute abdominal crises. The diagnosis in our case was difficult preoperatively due to the rarity of diverticula in the jejunum and in this age group. The patient also presented with non-specific complaints of hematochezia, shock, diffuse abdominal tenderness, and distension, which could mimic other acute abdominal conditions [5]. The more severe end of the spectrum of diverticular disease can present with complicated diverticulitis, perforation, and obstruction, all of which can have a significant impact on morbidity and mortality. Due to the possibility of diagnostic challenges posed by non-specific clinical presentation in relation to other acute abdominal conditions, a high index of suspicion is necessary, especially in elderly patients presenting with atypical abdominal symptoms or when conventional diagnostic modalities fail to elucidate the cause of abdominal distress [6].
Management revolves around clinical presentation and complications of jejunal diverticulosis. It is estimated that only 10%–40% of patients with jejunal diverticula are symptomatic [7]. Asymptomatic patients can be managed conservatively with a focus on measures to prevent complications. Most cases of uncomplicated diverticulitis are managed with antibiotic therapy and supportive care. Surgical intervention is the mainstay of treatment for complications such as perforation, obstruction, or uncontrolled hemorrhage, though there have been cases of successful non-operative management in contained perforations [8]. Surgical treatment involves segmental resection with primary anastomosis and it can be done via laparoscopic approach or via exploratory laparotomy. Laparoscopic surgery may provide reduced postoperative morbidity and shortened length of hospital stay compared with exploratory laparotomy, although in massive diverticula and unclear diagnosis, laparoscopy’s role would be limited [9].
Conclusion
Jejunal diverticulosis is a rare condition with variable presentations with a wide range of severities. The care of patients with jejunal diverticulosis will depend largely on the clinical manifestations of the disease. This case report highlights the importance of considering this diagnosis in the evaluation of acute abdomen and the potential for manifestation in younger age group. Giant jejunal diverticula may have a similar clinical and radiographic presentation as toxic megacolon and should be included in the differential as a rare cause of abdominal pain and hematochezia. Further research on pathogenesis and treatment outcomes on jejunal diverticulosis will result in optimization and standardization of care for this uncommon disease.
Conflict of interest statement
None declared.
Funding
None declared.



