-
PDF
- Split View
-
Views
-
Cite
Cite
Steven L Zhang, Benjamin Z W Chung, Hui Wen Ng, Arterial occlusion secondary to prior cardiac catheterization in a radial forearm flap—lessons learnt from an unusual case, Journal of Surgical Case Reports, Volume 2024, Issue 6, June 2024, rjae391, https://doi.org/10.1093/jscr/rjae391
Close - Share Icon Share
Abstract
The radial forearm free flap (RFFF) is a workhorse flap for head and neck reconstruction. We present an unusual case of radial artery occlusion, likely from previous transradial cardiac catheterization, in a patient for whom an RFFF was raised for floor of mouth reconstruction following resection of squamous cell carcinoma. Pre-operative assessment with ultrasound Doppler and an Allen test was normal. The flap was raised uneventfully under tourniquet control. However, following flap elevation and tourniquet release, poor flap perfusion was noted, and cutback of the artery revealed a long segment of hard fibrous plaque within the lumen. Retrospective review of medical records showed a history of cardiac catheterization via the same radial artery. We discuss various measures that can prevent this occurrence, including careful pre-operative screening of previous procedures involving the radial artery, the reverse Allen test, Doppler ultrasound, and consideration of distal arterial exploration without a tourniquet.
Introduction
The radial forearm free flap (RFFF) is a workhorse flap in head and neck reconstruction [1, 2]. Although rarely described, its viability may be compromised by radial artery occlusion (RAO) secondary to transradial coronary catheterization [3]. We report an unusual case of RAO which was noted following RFFF harvest. Retrospective review of medical records revealed a history of transradial cardiac catheterization, which was likely to be the cause. We discuss various measures that can help prevent this occurrence.
Case report
A 73-year-old chronic smoker underwent attempted RFFF reconstruction following resection of a floor of mouth tumour. Pre-operatively, Allen test and reverse Allen test were normal. The radial pulse was palpable, and bedside Doppler ultrasound showed positive signals, though weaker at certain points. The right radial artery was chosen as the patient was hemiplegic from a previous stroke 8 years ago and reliant on his left upper limb. The flap was raised uneventfully under tourniquet control.
However, following tourniquet release, there was poor flap perfusion, with an abrupt cut-off of pulsation and indocyanine green uptake at the mid-pedicle, 10 cm proximal to the skin paddle. The artery was sequentially cutback from proximal to distal (Fig. 1), and a point of resistance was noted on attempted advancement of a flushing cannula at the cut-off point (Video S1). Subsequent cutback revealed a long segment of hard fibrous plaque within the lumen (Fig. 2). The flap was abandoned and a pectoralis major flap was used for reconstruction instead. The patient made an uneventful recovery thereafter.
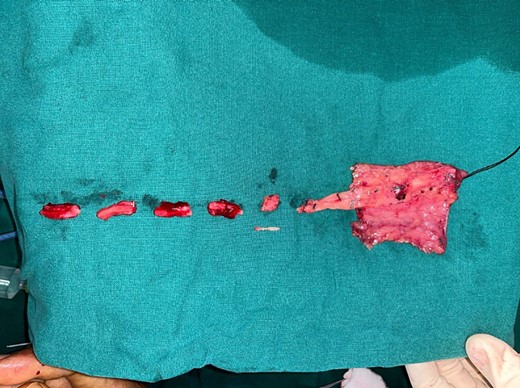
Sequential cutback of the radial artery, showing hard fibrous plaque starting from around 10 cm proximal to the skin paddle.
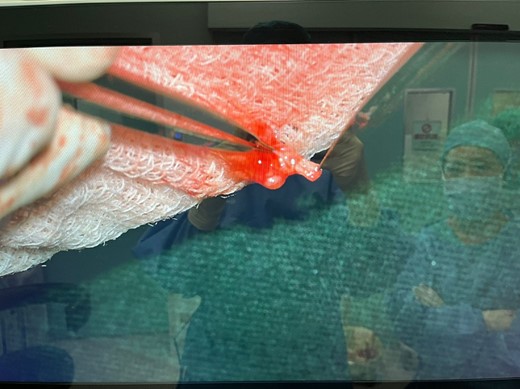
Microscopic view of fibrous plaque within the lumen of the radial artery.
On retrospective review of records, it was noted that the patient had undergone cardiac catheterization 8 years prior with right transradial artery access, which we attributed as the likely cause of occlusion.
Discussion
RAO may result from percutaneous cannulation [4], especially for cardiac catheterization [5], where the transradial route is becoming increasingly used [3]. This is common in head and neck cancer patients, who often have a history of smoking [6] and associated coronary artery disease.
Studies examining the use of the radial artery as a coronary artery bypass graft (CABG) have shown evidence of structural and functional damage to the arterial wall following cardiac catheterization [5, 7]. As compared with CABG, there are surprisingly few reports on the impact of cardiac catheterization on the RFFF [8]. Foreman et al. [9] reported a case of RAO caused by previous intra-arterial catheter insertion. In contrast, the location of occlusion in our case was 10 cm proximal to the skin paddle, beyond the reach of a standard intra-arterial cannula, hence the aetiology of injury was more likely from cardiac catheterization, which may cause trauma to any part of the radial artery [10].
de Bree et al. [8] and Chang et al. [11] reported cases of RAO caused by atherosclerosis rather than prior instrumentation, as evidenced by the presence of atherosclerotic plaques. This is uncommon, as studies have shown that in patients undergoing CABG, only 1% have severe stenosis of >40% in the radial artery [12], and that the lumen size is usually large enough to permit reasonable flow even in advanced disease [13]. In our patient, given the history of cardiac catheterization, and that the rest of the radial artery proximal to the point of occlusion did not have calcifications or atherosclerotic plaques, the cause of occlusion was most likely due to previous cardiac catheterization rather than atherosclerosis.
Another possible contributory factor for RAO in our patient was the hemiplegic status of his upper limb. Limited studies suggest that paralysed limbs of stroke patients have lower arterial extensibility compared with the non-paralysed side [14], and an ongoing study aims to evaluate the changes in pulse waves of the radial artery on the paralysed side of hemiplegic patients [15]. However, these studies only aim to assess if the pulse waveforms can be used to evaluate the result of stroke treatment, rather than any effect on arterial occlusion. Further studies are required to ascertain if hemiplegia has any correlation with RAO.
In our case and the other reports discussed above, pre-operative clinical assessment of the radial pulse and Allen test alone were insufficient to detect RAO. This is because there is often collateral circulation to the radial artery from the ulnar artery via the palmar arches [11]. de Bree et al. [8] and Foreman et al. [9] suggest performing the reverse Allen test to assess for flow via the radial artery with the ulnar artery occluded. In our case the reverse Allen test was noted to be normal. Possible explanations could include poor technique (for instance insufficient pressure when occluding the ulnar artery) or aberrant collaterals between the ulnar and radial arteries. Doppler ultrasound may be more useful, but only if the entire course of the artery is examined [11]. In our case, Doppler ultrasound showed positive signals but certain points had weaker signals. In retrospect, this should have been interpreted as a sign of possible segmental arterial occlusion.
Based on our experience from this case, we suggest the following measures be taken whenever an RFFF is considered:
(1) A thorough history and review of medical records should be performed to screen for previous transradial cardiac catheterization, and if present that side should be avoided. Of note, RAO may be persistent even many years after cardiac catheterization, with some studies showing a progressive deterioration in radial artery function over time [5].
(2) In addition to the Allen test, the reverse Allen test should also be performed to assess for radial artery patency [9]. Proper care should be taken to ensure sufficient and constant pressure on the ulnar artery upon release of the radial artery, to reduce the chance of a false negative result.
(3) Doppler ultrasound should be performed along the entire course of the radial artery, and any reduction in signal intensity or pattern should be interpreted as a sign of possible arterial occlusion.
(4) If there is any concern of radial artery patency based on pre-operative assessment, then the flap elevation technique can be modified: prior to tourniquet inflation, the artery can be explored first through the distal incision, and divided between vessel clamps to allow for assessment of pulsatility and flow; should these be inadequate, the artery can then be repaired and a different donor site chosen instead. This will minimize donor site morbidity and unnecessary wastage of operative time.
In conclusion, RAO is a potential complication of cardiac catheterization which compromises the usage of an RFFF. While there are limited reports of this phenomenon, it is probably more common in practice, as can be inferred from the numerous studies pertaining to CABG. The lessons learnt from our experience may help reconstructive surgeons avoid a similar situation.
Conflict of interest statement
None declared.



