-
PDF
- Split View
-
Views
-
Cite
Cite
Isha Gupta, Elliott Moussa, Karun Motupally, Sharon Morris, Diagnosis of an unusual orbital abscess following sub-Tenon's steroid injection: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjae339, https://doi.org/10.1093/jscr/rjae339
Close - Share Icon Share
Abstract
Orbital abscesses are caused by infection within or near the orbit and show obvious signs of pain, proptosis and raised inflammatory markers. Diagnosis is based on clinical features and radiological imaging, and requires early antibiotics and often surgical drainage to save vision. Sub-Tenon’s injections of triamcinolone acetonide (TA) have caused localized infections in previous reports, which have responded to therapeutic interventions. Here we report a case where a delayed presentation of an orbital abscess secondary to sub-Tenon’s TA for persistent post-operative cystoid macular oedema, without obvious signs of infection, rapidly progressed to cause orbital compartment syndrome. Despite treatment, the patient lost complete vision in the affected eye. This case discusses the rare and unusual cause of abscess formation and a diagnostic dilemma.
Introduction
Orbital abscesses are a notable complication of orbital cellulitis, and prompt treatment with intravenous antibiotics and drainage allows optimal visual recovery. Here we report the case of a patient with no known history of diabetes or sinusitis, who received a sub-Tenon’s injection of triamcinolone acetonide (TA) 4 months prior. Initial radiographic imaging showed an inflamed intraconal epithelial-lined cyst in the right orbit, which rapidly progressed to orbital compartment syndrome and subsequent complete vision loss, despite therapeutic measures. A review of the literature identified seven reports of orbital abscesses attributed to TA injections, with three associated with Staphylococcus aureus infections. The delayed onset of symptoms complicated diagnostic efforts, highlighting the inherent challenges in management.
Case report
An 83-year-old male presented to emergency following a referral from his private ophthalmologist. He had a 2-week history of severe right eye pain, conjunctival injection, mildly decreased visual acuity, and some restriction in extraocular movement, and notably increased proptosis compared to an assessment 3 days prior. Eye pressures and fundal examination were normal. The patient’s ocular history included bilateral cataract surgery, requiring subsequent interventions including ex-plantation and replacement with an anterior chamber lens due to pseudophakic opacification in the right eye, and right eye retinal detachment requiring vitrectomy and management of post-operative epiretinal membrane formation and refractory cystoid macular oedema (CMO). This was managed with intravitreal steroid injections (Ozurdex). Notably, he had received a single dose of 40 mg sub-Tenon TA injection four months prior for persistent CMO.
Preceding this presentation, magnetic resonance imaging (MRI) attributed his presenting features to an inflamed retroorbital congenital cystic structure, adjacent to the inferonasal aspect of the globe, accompanied by mild inflammatory changes in the surrounding orbital tissues. At the time, this was considered radiologically not infective (Fig. 1). He was afebrile, without raised inflammatory markers. Whilst pending further diagnostic opinion, a trial of oral steroids was given. He had clinically improved within the month of commencing treatment with reduced inflammation.
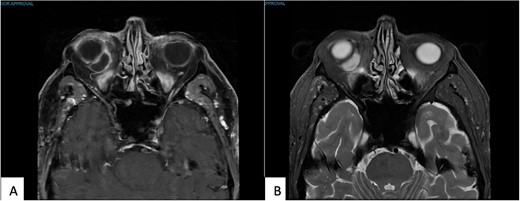
(A) T1 MR Orbits, and (B) T2 MR Orbits shows an intraconal mass measuring 16 × 8 × 15 mm in the inferonasal quadrant abutting the wall of the globe in the right orbit.
However, on tapering the steroids the patient relapsed and re-presented to emergency exhibiting severely compromised vision limited to vague light perception, reverse relative afferent pupillary defect, elevated intraocular pressure measuring 50 mmHg, complete ophthalmoplegia, and oedematous eyelids with conjunctival injection and chemosis of the right eye (Fig. 2). Slit lamp examination showed no signs of intraocular infection or inflammation. Initial management included administration of topical aqueous suppressants and intravenous acetazolamide, emergent bedside lateral canthotomy and inferior cantholysis and concurrent aggressive systemic antibiotic therapy, comprising flucloxacillin, ceftriaxone, and metronidazole. A swab of the anterior ocular surface yielded growth of methicillin-sensitive S. aureus. Subsequent administration of high-dose intravenous steroids, coupled with initial therapies resulted in improvement of vision to vague hand movement perception and pressure at 4 mmHg.

Appearance of right eye orbital compartment syndrome secondary to acute progression of the orbital abscess.
Computed tomography imaging (Fig. 3) showed a 11 × 15 × 14 mm peripherally enhancing collection at the posteroinferior aspect of the right globe concerning for an orbital abscess or infected orbital cyst, with associated retroorbital fat stranding and thickening of the lateral rectus.
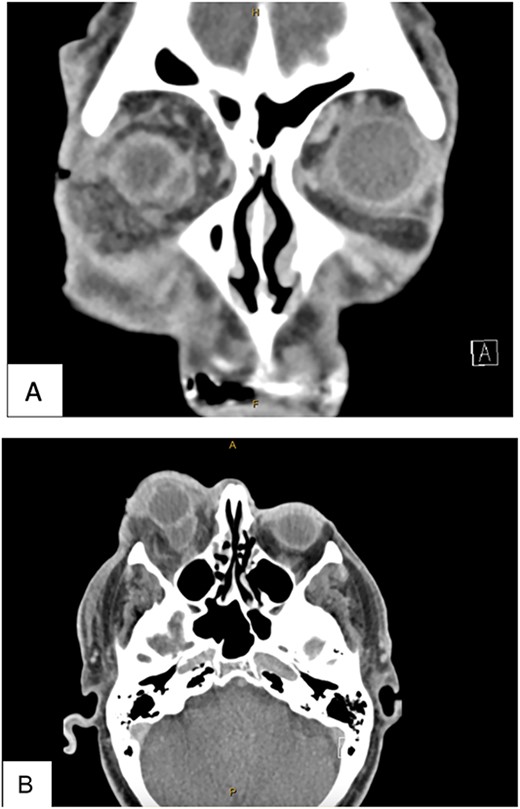
This CT was taken post lateral canthotomy. (A) CT Head with Contrast Coronal View. (B) CT Head with contract axial view. Both views show an 11 × 15 × 14 mm peripherally enhancing collection abutting the posteroinferior aspect of the right globe. There is associated retrobulbar fat stranding. There is thickening and enhancement of the lateral rectus muscle. The right optic nerve sheath shows enhancement but no signs of effusion.
The patient underwent transconjunctival peritomy and drainage of the inferomedial abscess. However, vision regressed from hand movements to no light perception 5 days following initial drainage. Re-imaging of the orbit revealed a new retroorbital abscess accumulation superior-temporally (Fig. 4) that was also then drained. Both collections contained frank pus, and cultures also grew methicillin sensitive S. aureus, requiring a prolonged course of intravenous flucloxacillin and oral steroids. Subsequent MRI showed right lateral retroorbital abscess regression and less prominent retroorbital phlegmonous changes (Fig. 5). However, vision did not return to the patient’s eye.
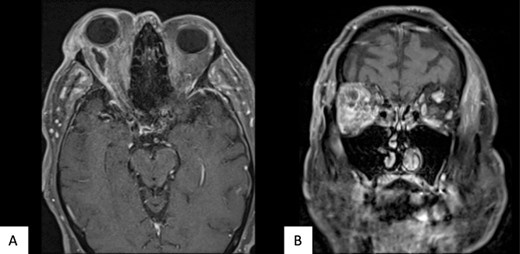
Axial (A) and coronal (B) MRI T1 FS post contrast imaging demonstrating new, right sided posterosuperior, peripherally enhancing collection post drainage of previous collection.
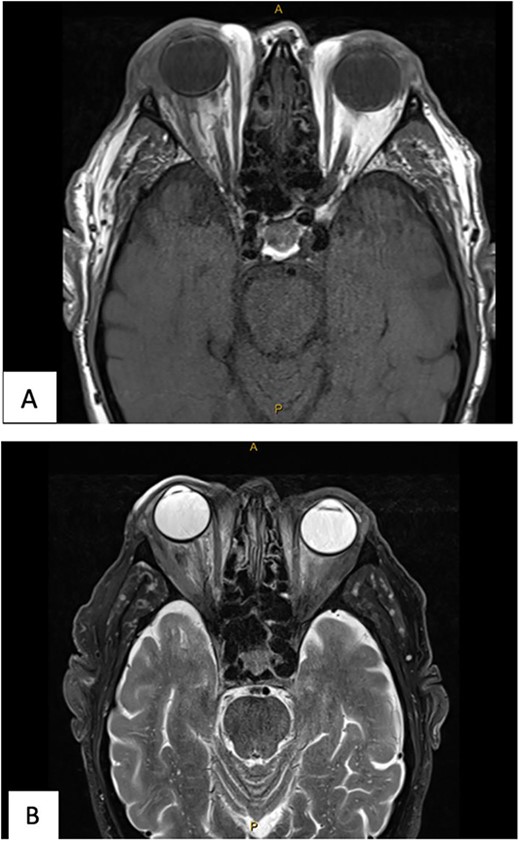
(A) MR Orbit T1 TSE R TRA. (B) MR Orbit T2 FS TSE TRA. The right lateral retroorbital abscess has reduced in size. The traction on the optic nerve has reduced.
Discussion
Orbital abscesses are not a well-recognized complication of TA injections with only seven reports in literature reporting this [1]. Four reports cultured fungal content including Aspergillus flavus, Exophiala dermatitidis, Scedosporium apiospermum, and Pseudallescheria boydii, respectively [2–5]. These abscesses had a substantially delayed presentation, occurring months after injection [2–5]. Although delayed, three cases had obvious infective signs, allowing for timely treatment and some visual recovery [2, 4, 5]. The remaining three reports grew S. aureus [6–8]. In one case the patient presented with infective signs 6 weeks post injection [6]. In the other cases, only 3 weeks transpired between injection and presentation [7, 8]. All three cases presented with clear signs of orbital cellulitis and imaging showed obvious abscess formation, allowing for timely treatment and good visual recovery [6–8]. In all seven case reports the infections occurred in individuals with diabetes or on long term steroid treatment [2–8].
There are two articles describing orbital abscesses masquerading as benign cysts in adult patients; these cases involved patients with tuberculosis, dental infections [9], and a mucocele that slowly progressed into an orbital abscess [10]. To our knowledge this is the only case of an orbital abscess caused by a TA injection four months prior masquerading as an orbital cyst, and no known history of prior infection in an adult patient. On imaging, orbital abscesses present similarly to orbital cysts as both are peripherally enhancing lesions differentiated by clinical features, namely proptosis, change in vision, ophthalmoplegia and signs of infection [11].
Other than the patient’s refractory post-operative CMO requiring the TA injection, this patient exhibited no other risk factors for orbital abscess development. However, there were a few contributing factors that led to diagnostic confusion in this case. On initial presentation, the position of the collection being very posterior likely masked anterior orbital infective features. Also, the patient was initially responsive to oral steroids and did not show systemic features of infection. The combination of localized sub-Tenon’s injection and systemic steroids likely dampened immunologic response to the infective agent, temporarily reducing surrounding inflammation until the collection later progressed causing compartment syndrome.
Sub-tenon TA injections are common procedures that rarely cause infective complications, as povidone-iodine preparation and aseptic technique while injecting are usually sufficient to prevent contamination of the sub-Tenon’s space. Yet, this case demonstrates that abscesses can occur and present late following TA injections. Orbital infections should be suspected early in all orbital cystic masses, particularly those with a potential seeding incident as they require timely antibiotic treatment and potential surgical drainage for good visual outcomes [12].
Conflict of interest statement
The authors have no conflict of interest.
Funding
The authors have not received any external funding for this study.



