-
PDF
- Split View
-
Views
-
Cite
Cite
Anupama Barua, Prakash Nanjaiah, Richard Warwick, Ravish Jeeji, Lognathen Balacumaraswami, A customized technique for confluent aortic annular and selective sinus of Valsalva endocarditis, Journal of Surgical Case Reports, Volume 2024, Issue 2, February 2024, rjae089, https://doi.org/10.1093/jscr/rjae089
Close - Share Icon Share
Abstract
We describe a novel technical modification for reoperative aortic valve replacement in destructive recurrent prosthetic aortic valve endocarditis. We encountered complex anatomy in a previously operated aortic root wherein the aortic annulus and the right coronary sinus of Valsalva were destroyed. This precluded secure suture placement. We modified a composite mechanical Valsalva conduit to create a separate sinus of Valsalva left in continuity with the mechanical valve. This approach allowed us to exclude the infected right sinus of Valsalva and the corresponding aortic annulus.
Introduction
Prosthetic aortic valve endocarditis with destruction of aortic valve and annulus extending into the sinus of Valsalva is an unusual and frequently fatal complication. The surgical management is challenging. Mortality after surgical intervention ranges from 23% to 40% [1, 2]. Radical surgical debridement of the infected tissue is essential for preventing recurrent endocarditis. Paucity of healthy aortic tissue following debridement of the infected materials presents a technical challenge. Abscess formation in sinus of Valsalva is a very complex problem and there is lack of robust literature for guiding appropriate management. We report a novel technique for a tailored repair of sinus of Valsalva with confluent aortic valve replacement by excluding the infected material without aortic root replacement.
Case report
Cardiopulmonary bypass was instituted using peripheral cannulation. Redo median sternotomy was performed after decompressing the ascending aorta. The patient was cooled to 28°C. Retrograde cardioplegic arrest was established and an extended oblique aortotomy was performed to obtain good exposure of the infected root. This revealed that the prosthetic aortic valve was dehisced along the anterior half of the circumference with significant out pouching of right coronary sinus where the old pericardial patch was attached during previous surgery for infective endocarditis. Old glue residues were carefully removed. Diligent debridement was carried out. The prosthetic valve was carefully excised and annulus was debrided. After meticulous resizing, a 25 mm Carboseal Valsalva mechanical prosthetic graft with an inverted U shaped leaf of Dacron cut out from the valves conduit was prepared (Fig. 1). It was sutured in the supra-annular position using intermittent pledgeted 2′0″ Ethibond sutures in a horizontal mattresses fashion. The right coronary sinus was reconstructed using the inverted ‘U’ shaped Dacron leaf patch excluding the sinus and cavity around the right coronary annulus area using 5′0″ polypropylene continuous sutures (Fig. 2). The aorta was closed in layers.
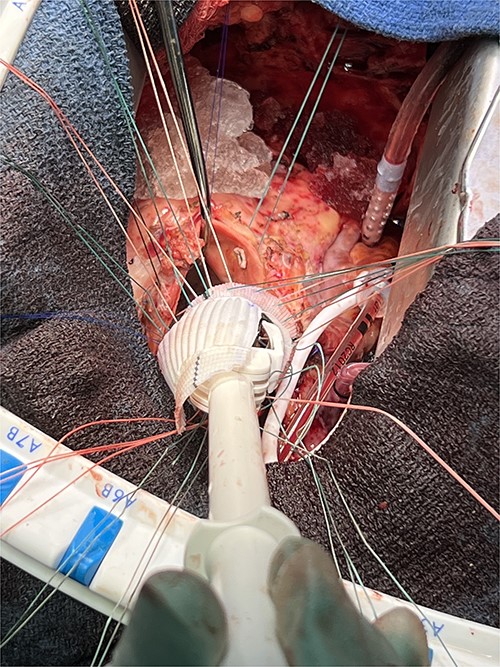
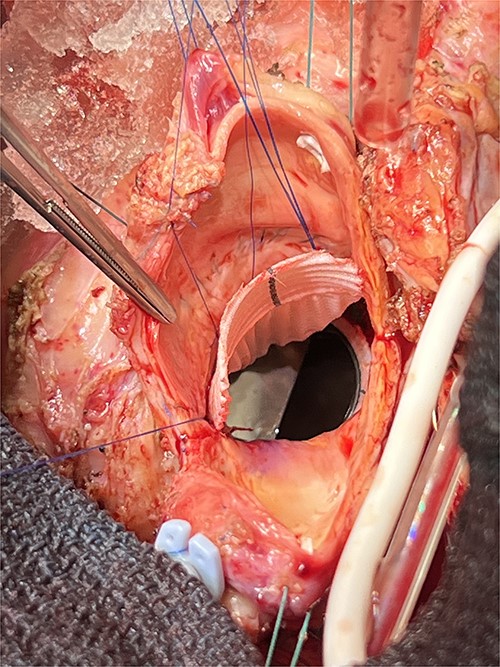
The composite graft implantation in aortic position with Dacron patch in situ.
On table, transoesophageal echocardiography (TOE) demonstrated well-seated and functioning aortic mechanical prosthesis without any leak around the Dacron patch.
Discussion
We used this modified technique in a 56 years old man who had recurrent infective endocarditis involving the aortic annulus with abscess formation around the right coronary sinus of Valsalva. Because of the extension of the abscess in the sinus of Valsalva, we decided to use the composite graft with inverted ‘U’ shaped leaf of the graft as a patch to exclude the cavity allowing us to avoid the use of pericardial patch and the complete aortic root replacement. Preoperative TOE revealed paravalvular leak with severe aortic regurgitation and dilated aortic root. Intraoperative TOE after repair of sinus of Valsalva revealed no paravalvular leak and no leak around the Dacron patch at the right coronary sinus of Valsalva.
Many authors used different techniques to repair the defect in sinus of Valsalva for infective endocarditis. Extensive tissue destruction of the aortic annulus made the surgical technique challenging. Reconstruction of the sinus by pericardial patch was demonstrated by several authors [3]. Modified Bentall procedure or aortic root replacement could be used in this situation which is more challenging due to lack of healthy tissue [4, 5]. However we did follow that way of repairing the sinus as there was no healthy tissue to hold the sutures safely. This technique required less sutures and it was easier to hold the annulus. Therefore, we approached this technique to exclude the abscess cavity from the surgical field.
Author contributions
AB: conception or design of the work, data collection and interpretation and drafting the article; PN: critical review; RW: critical review; RJ: critical review and LB: critical review, final approval.
Conflict of interest statement
None declared.
Funding
None declared.



