-
PDF
- Split View
-
Views
-
Cite
Cite
Daisuke Yamashita, Kazuta Yamashita, Kosuke Sugiura, Masatoshi Morimoto, Hiroaki Manabe, Fumitake Tezuka, Koichi Sairyo, Robotic-assisted minimally invasive repair surgery for progressive spondylolysis in a young athlete: a technical note, Journal of Surgical Case Reports, Volume 2024, Issue 2, February 2024, rjae085, https://doi.org/10.1093/jscr/rjae085
Close - Share Icon Share
Abstract
Presently, the invasiveness of direct repair surgery for lumbar spondylolysis is relatively high. Thus, high school and junior high school students who play sports often cannot return to sports before graduation because of the invasiveness. The use of a robotic system enabled an accurate and minimally invasive procedure. Robotic-assisted minimally invasive direct pars repair surgery is useful for young patients with progressive spondylolysis.
Introduction
Lumbar spondylolysis usually occurs in children and adolescents who are active in sports and causes low back pain [1]. The cause of spondylolysis in these patients is thought to be repetitive stress on the pars interarticularis with subsequent microfracture [2]. Sairyo et al. reported that lumbar spondylolysis can be divided to three stages: early, progressive, and terminal [3].
The treatment plan depends on the disease stage and the patient’s background. In general, conservative treatment is the first choice, but surgical treatment is chosen in patients who are at risk of pseudoarthrosis or who hope for reliable bone union and a quick recovery. Most athletes who undergo surgery hope for minimal invasiveness, but spondylolysis repair surgery sometimes requires major damage to the posterior muscle. Following spondylolysis repair surgery, high school and junior high school students who play sports often cannot return to sports before graduation because of the invasiveness. Thus, they tend to opt for conservative treatment in order to continue playing sports regardless of the bone union.
Recently, robotic assistance has been introduced into spine surgery, allowing for an accurate insertion of pedicle screws even in small and deformed pedicles. We apply this robotic system to spondylolysis repair surgery. In this paper, we report the case of 16-year-old boy with progressive spondylolysis who underwent robotic-assisted minimally invasive surgery.
Case report
The patient was a 16-year-old boy, a javelin thrower. When throwing the javelin, he experienced severe low back pain and visited a nearby hospital. He had low back pain during extension of the lower spine. Plain radiographs showed pars fracture at L3. Despite stopping sports activity and wearing a hard brace for 6 months, he still had pain and was referred to our hospital. CT scans showed a complete fracture line, and T2-weighted MRI showed a high signal in the pedicles bilaterally (Fig. 1). We diagnosed progressive spondylolysis at L3. He strongly hoped for an early return to sports activity, and we scheduled surgical treatment.
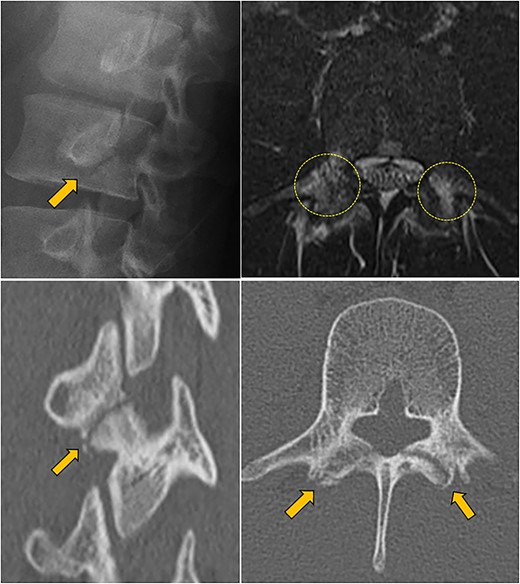
Preoperative lumbar X-ray, MRI, and CT scan; upper left: oblique view X-ray showed a complete fracture line (arrow); upper right: horizontal T2-weighted MRI showed a high signal area in the pedicles bilaterally (circles); lower left, right: oblique and horizontal CT scan showed a complete fracture line in the pars (arrow).
Surgical techniques
The procedure was divided into two mains phases, namely, navigation and fixation.
Navigation phase
The patient was placed prone on a carbon spine frame. A central skin incision was made over the spinous process at L2 (15 mm in length). A reference antenna with infrared light ball was set at the L2 spinous process and a tungsten marker was placed on the skin. The affected spinal bone structure was input into the navigation system using an intraoperative CT scan (O-arm, Medtronic). The best skin incision point was decided by checking the navigation monitor.
Fixation phase
Skin incisions for screw insertion were made bilaterally (each 10 mm in length). The fascia and paravertebral muscles were cut for screw insertion. The screw insertion point, insertion angle, and screw length were planned using the navigation pointer and were registered in the navigation system (Fig. 2). The robotic arm was moved manually to a position near the target point, and it then automatically moved to the planned point precisely. The canula was inserted though the robotic arm, and the screw trajectory was made using a power drill (Fig. 3). After drilling, the guidewire was inserted into the drilled hole and tapping was performed through the guidewire. Finally, the planned screws were inserted via the guidewire. The screw position was confirmed by fluoroscopy and postoperative X-ray. Each wound was washed and closed without a drain tube (Fig. 4). There were no intraoperative complications.
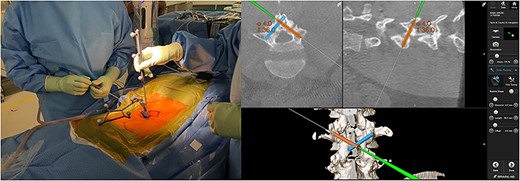
Screw planning; the appropriate screw length and angle were displayed on navigation monitor (right panel).
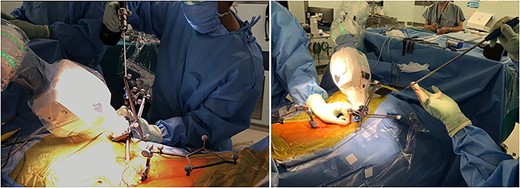
Making screw hole using a power drill with robotic arm (left panel); insertion of screw via a guidewire (right panel).

Postoperative management
The postoperative course was uneventful, and he did not complain about low back pain. He started to walk 1 day after the surgery wearing a hard trunk brace. Jogging was allowed 1 month after the surgery. Two months after the surgery, CT scans showed sufficient bone union and he started sprinting and twisting his lower spine (Fig. 5). Finally, he returned to javelin throwing without any pain and took part in a national competition 12 months after the surgery.
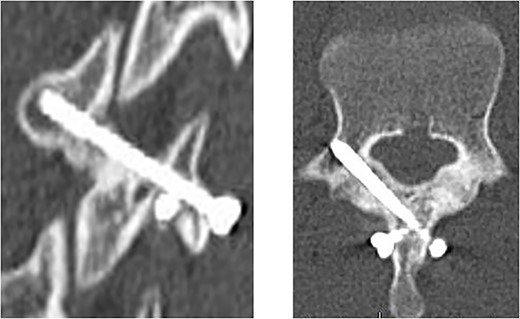
CT scan at 2 months after surgery; oblique view (left panel) and horizontal view (right panel).
Discussion
In this case, we encountered a 16-year-old boy with progressive spondylolysis who underwent robotic-assisted minimally invasive surgery and had a favorable postoperative course. This is the first report to describe the robotic-assisted direct pars repair surgery for spondylolysis.
Direct spondylolysis repair surgery has been performed to treat chronic low back pain in young patient without slippage and disk degeneration. Several repair techniques have been reported [4–7]. The clinical outcomes are satisfactory, but some methods require advanced technical skills [8–10]. An open repair surgery usually requires a large skin incision and muscle division to insert the screw correctly. Back muscle degeneration after the surgery is extremely undesirable for athletes. Despite the invasiveness of this approach, it is sometimes quite difficult to insert the screw at the optimal position because the pars is a thin, small target. Surgeons might hesitate to choose spondylolysis repair surgery because of its difficulty and high invasiveness.
Robotic-assisted minimally invasive surgery can solve these two major problems. This technique requires small skin incisions for navigation and screw insertion. Also, it is not difficult to detect the correct screw insertion point and angle and to insert a screw through a small skin incision via a guidewire. Furthermore, using a navigation system, the surgeon can easily choose the appropriate screw length and can avoid occupational radiation exposure to medical staff. We believe this technique can be useful for low back pain due to spondylolysis in young athletes who have a low likelihood of natural bone union with conservative treatment. However, this method is not indicated for spondylolysis in the terminal stage, which requires decortication of the pars defect and bone grafting in order to achieve bone union. For isthmic spondylolisthesis and terminal spondylolysis, the PS-hook rod method or smiley face rod method is a reasonable option [11, 12].
Robotic-assisted surgery has many benefits, such as accurate surgical planning, low invasiveness, high screw accuracy, and low radiation exposure for medical staff [13]. However, it also has some shortcomings, such as the high cost of the infrared ball of the navigation system and the sterilized nylon cover of the robotic arm. Nonetheless, robotic surgery seems very effective for the direct repair of progressive spondylolysis. Sairyo et al. reported that the union rates of conservative treatment for spondylolysis in the progressive stage was relatively low, even in younger patients [14]. The union rate was 27%–64%, and the time to bone union was 5.4–5.7 months. Robotic-assisted minimally invasive direct pars repair surgery can be considered in cases of progressive spondylolysis where the patient hopes for reliable bone union and an early return to sports.
In summary, robotic-assisted minimally invasive direct pars repair surgery is useful for young patients with progressive spondylolysis.
Limitation
As this is a case report and technical note that showed the utility of the robotic system and how to insert the screw to pars fracture site, complications and functional results need to be investigated in a case series or a case–control study.
Conflict of interest statement
None declared.
Funding
None declared.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.



