-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammed F Shaheen, Faisal J Almalki, Abdulrahman Altheaby, Bader Alsaikhan, An unusual hernia postkidney transplantation led to intermittent ureteric obstruction, Journal of Surgical Case Reports, Volume 2024, Issue 2, February 2024, rjae060, https://doi.org/10.1093/jscr/rjae060
Close - Share Icon Share
Abstract
A 53-year-old man underwent a living donor kidney transplantation in the right iliac fossa 25 years prior to presentation. He had been noting an inguinal bugle that became more prominent as the day progressed, and it regressed at night. Upon further investigations, an ultrasound of the allograft revealed moderate-to-severe hydronephrosis. A computed tomography scan revealed herniation of the bladder and part of the transplanted ureter within the supravesical/direct inguinal space. Lichtenstein-like fashion of repair was performed, and the patient continues to enjoy satisfactory graft function with no recurrence. The case illustrates a rare hernia as a late complication of the kidney transplant incision leading to ureteric obstruction and a successful attempt at operative repair.
Introduction
A hernia is defined as a protrusion, bulge, or projection of an organ or part of an organ through the body wall that normally encloses it [1]. Pregnancy, weightlifting, constipation, and weight gain are well-known risk factors for hernia [2]. Supravesical hernia is a rare type of hernia that occurs in the supravesical fossa between the median and the medial umbilical ligaments. Only a few cases in the literature report supravesical hernias leading to hollow viscus obstruction. We report a case of an unusual manifestation of supravesical hernia that developed years postkidney transplant and resulted in episodic ureteric obstruction leading to hydroureteronephrosis.
Case report
A 53-year-old man, who underwent a living donor kidney transplantation in the right iliac fossa in 1996, presented to the post-transplant clinic for regular follow-up.
Despite a new onset proteinuria of 50 mg/dl, he continued to have a good functioning graft with a creatinine level of 93 μmol/l corresponding to an estimated glomerular filtration rate (eGFR) of 78 ml/min/1.73 m2. Nonetheless, he had also been noting an inguinal bugle that becomes more prominent as the day progressed, and it regressed at night. Upon further investigations, an ultrasound of the allograft revealed moderate-to-severe hydronephrosis. Further imaging using computed tomography scan (CT) confirmed the presence of upstream moderate hydronephrosis (Figs 1A and2A) along with a reported herniation of the ureter in a right inguinal hernia, resulting in a focal distal ureteric dilatation of 3.5 cm (Fig. 3A).
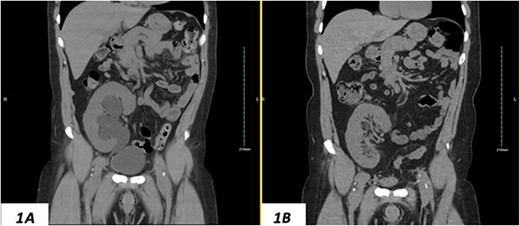
(A) Hydronephrosis of the allograft ureter on preoperative coronal CT scan; (B) significant improvement of hydronephrosis on the 10-month postoperative image.
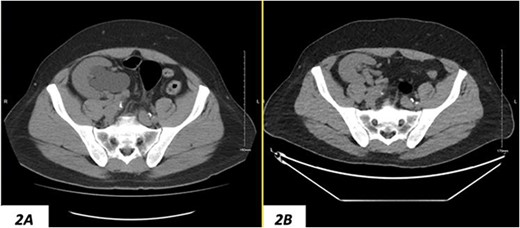
(A) Hydronephrosis of the allograft ureter on preoperative cross-sectional CT scan; (B) significant improvement of hydronephrosis on the 10-month postoperative image.
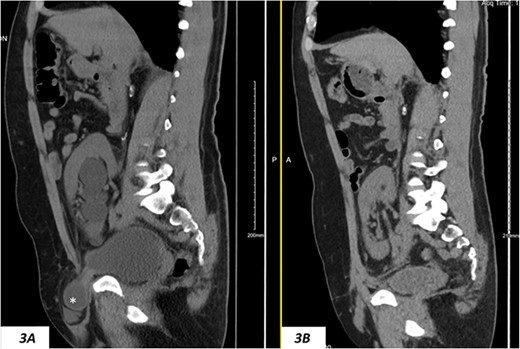
(A) Hydronephrosis on preoperative sagittal CT scan showing the reported dilated part of the distal ureter (*), which was correctly identified intraoperatively as a sliding dome of the bladder; note the relationship to the pubic bone; (B) significant improvement of hydronephrosis on the 10-month postoperative image.
After counseling the patient about the findings, a surgical intervention was planned aiming at fixing the inguinal hernia and potentially reimplanting the ureter after resection of the reportedly ectatic part of the ureter.
The patient underwent surgical repair in June 2022. Intraoperative findings revealed a sliding supravesical hernia with an elongated and redundant bladder dome—where the ureteric anastomosis resides—rather than a dilated ureter per say. The dome of the bladder was noted to slide into the hernia when the bladder was filled, which seems to be the mechanism leading to intermittent ureteric obstruction, explaining the observed hydronephrosis without obvert deterioration of kidney function. The epigastric vessels were not identifiable; however, the spermatic cord was coursing at the lateral edge of the hernia sac and the rectus sheath fascial defect extended to the pubic tubercle inferomedially with the rectus muscle pushed to the midline. The hernia location resembled a supravesical hernia. Therefore, a planned repair of the hernia was planned without further interruption of the allograft or the ureteric anastomosis.
The surgical repair aimed to re-establish the inguinal canal posterior wall, which was done by approximating the edge of the anterior rectus sheath to pubic tubercle and the reflecting edge of the inguinal ligament. This was followed by the application of light polypropylene mesh in Lichtenstein-like fashion of repair (Fig. 4) allowing the spermatic cord structures to course anterior to the mesh. An approximation of the conjoint tendon to the inguinal ligament was then performed over the spermatic cord to resemble the roof and anterior wall of the inguinal canal.
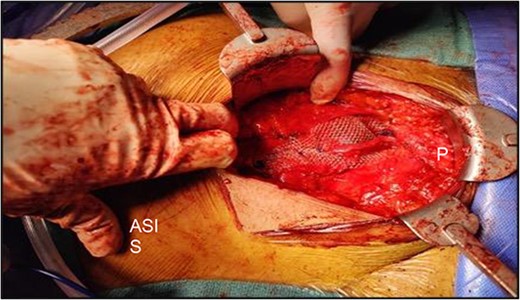
Intraoperative picture showing light polypropylene mesh in Lichtenstein-like fashion of repair; please note the relative location of the pubic bone (P) and the anterior superior iliac spine (ASIS).
The hydronephrosis significantly improved in the 1-year follow-up imaging (Figs 1–3B). The patient continues to enjoy satisfactory graft function with no hernia recurrence. As of July 2023, the patient had further improvement in graft function reflected via a serum creatinine of 76 μmol/l reflecting a eGFR of 99 ml/min/1.73 m2 and 10 mg/dl of proteinuria.
Discussion
Ventral abdominal hernia is a common surgical condition that can affect all ages and both genders [3]. Previous surgery, trauma, and repetitive stress on naturally weak regions of the abdominal wall are common causes of acquired ventral hernias [4]. Most of the incisional hernias are associated with open abdominal surgeries [5].
The vulnerability to develop a supravesical incisional hernias postkidney transplantation may be attributed to the anatomic and surgical factors associated with the procedure. A large incision, designed to provide optimal access to the transplant site, may inadvertently predispose the patient to fascial weaknesses, especially if the incision extends significantly in the inferiomedial direction toward the symphysis pubis.
The incidental discovery of an allograft ureteric obstruction due to a supravesical incisional hernia, as presented in this case, is a noteworthy finding. It underscores a critical need for care and monitoring in patients who have undergone kidney transplantation when they have peri-incisional complains [6]. This unique case highlights the need for vigilance in the postoperative period even long after surgery. Timely imaging studies to aid in early detection can have profound implications for patient morbidity and allograft survival.
This case also underscores the critical need for the careful evaluation of imaging studies and adopting cautious surgical strategy in the context of atypical clinical presentations. Such diligence is paramount in mitigating the risk of misdiagnosis, which can lead to suboptimal patient outcomes.
Conclusion
This reported case would be the first case to report allograft ureteric obstruction in a supravesical hernia in a patient who underwent kidney transplantation. Given the nature of the kidney transplant incision, patients may be prone to supravesical incisional hernias, particularly if the fascial incision extends generously in the inferiomedial direction above the pubic bone. Hence, a high index of suspicion in patients presenting with medial incisional bulge postkidney transplantation is needed to plan an appropriate repair.
Conflict of interest statement
None declared.
Funding
None declared.



