-
PDF
- Split View
-
Views
-
Cite
Cite
Adrian C K Chia, Junette Yu, Shaun Q W Lee, Nick Z P Ng, Lessons learned from a case of phlegmasia cerulea dolens treated with thrombolysis and iliac vein stenting, Journal of Surgical Case Reports, Volume 2024, Issue 12, December 2024, rjae773, https://doi.org/10.1093/jscr/rjae773
Close - Share Icon Share
Abstract
Phlegmasia cerulea dolens is a rare manifestation of massive deep vein thrombosis with threat to limb and life. A patient with a background of ovarian malignancy in remission and pelvic radiotherapy presented with left lower limb phlegmasia cerulea dolens as a result of extensive acute left lower limb deep vein thrombosis, extending from the popliteal vein to the inferior vena cava. While initial rapid thrombolysis and left iliac vein stenting were successful, she developed significant hemorrhagic complications from her right radial intra-arterial line with compartment syndrome requiring fasciotomy. She subsequently develops contralateral right lower limb deep vein thrombosis with phlegmasia cerulea dolens as a result of the cessation of anticoagulation and ‘jailing’ of the contralateral right iliac vein. Repeat thrombolysis with a lower dose of thrombolytics was performed, and contralateral iliac vein stenting in ‘kissing’ configuration was performed successfully. We discuss several lessons learned from this uncommon but important case.
Introduction
Phlegmasia cerulea dolens (PCD) is a rare cause of acute limb ischemia, typically arising due to massive ilio-femoral deep vein thrombosis (DVT). Known risk factors include malignancy, thrombophilia, surgery, trauma, inferior vena cava (IVC) filter, and radiotherapy. Timely diagnosis and intervention are critical to salvaging the limb before venous gangrene develops.
Case report
A 57-year-old lady presented with one day of left lower limb swelling and pain. On examination, her entire limb was swollen with bluish discoloration up to the thigh (Fig. 1). Dorsalis pedis and posterior tibial pulses were palpable, but capillary refill time (CRT) was delayed at 5 s. There was no numbness or weakness.

Three years ago, she underwent total hysterectomy, bilateral salpingo-oophorectomy, and bilateral pelvic nodal dissection, followed by adjuvant chemoradiotherapy for endometrial cancer. She was in remission at the presentation.
PCD was diagnosed clinically. A heparin bolus and infusion were administered immediately. Computed tomography (CT) angiogram confirmed DVT from the left popliteal vein to the distal IVC. The left deep femoral and internal iliac veins were also thrombosed.
Emergency IVC filter insertion, thrombolysis, and stenting were performed under general anesthesia in a hybrid operating suite. Via the right internal jugular vein, a retrievable IVC filter was deployed inferior to the right renal vein, after an on-table cavogram confirmed no thrombus involvement at that level. Pharmaco-mechanical thrombolysis (PMT) was performed using AngioJet Zelante (Boston Scientific, Marlborough, USA) and 20 mg of alteplase. The stenotic left iliac vein was then stented with Venovo 14 × 140 mm (BD Medical, Arizona, USA) and post-dilated with a Mustang 12 × 100 mm balloon (Boston Scientific, Marlborough, USA).
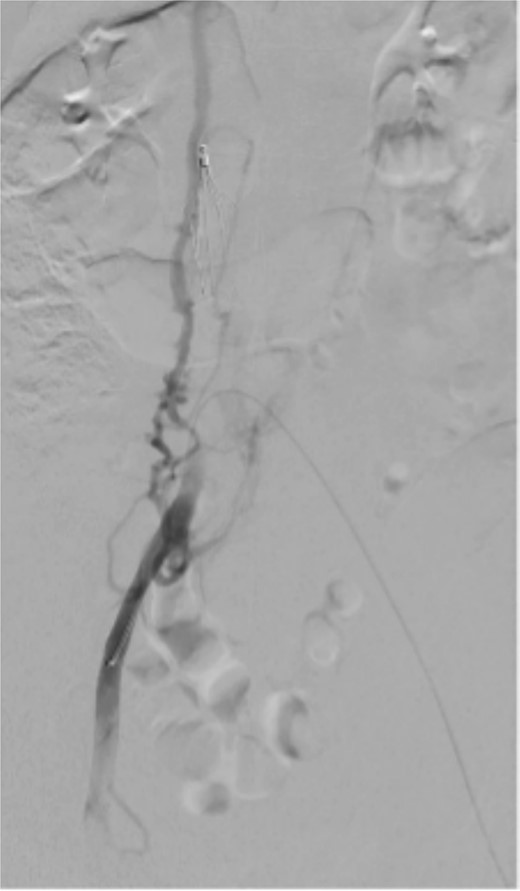
The completion venogram showed smooth contrast flow from the left popliteal vein upwards. The right common iliac vein was stenosed near the confluence, with a large collateral vein as the main outflow into IVC (Fig. 2). As outflow was thought to be adequate, no intervention was done on the right.
Postoperatively, the patient was maintained on a heparin infusion and subsequently converted to subcutaneous enoxaparin. Pneumatic calf compressors and thromboembolic deterrent stockings were applied.
Unfortunately, on postoperative Day 1, the patient developed right hand compartment syndrome due to a hematoma from the radial intra-arterial line. Hand fasciotomy and radial artery repair were performed, followed by wound debridement and closure on postoperative Day 9. Anti-coagulation was resumed immediately after each operation.
On postoperative Day 10, the patient complained of right lower limb swelling (Fig. 3). Ultrasound Duplex revealed acute thrombosis of her right common and external iliac veins. As pain and swelling increased overnight with prolonged CRT to 4 s, she underwent thrombolysis and stenting.

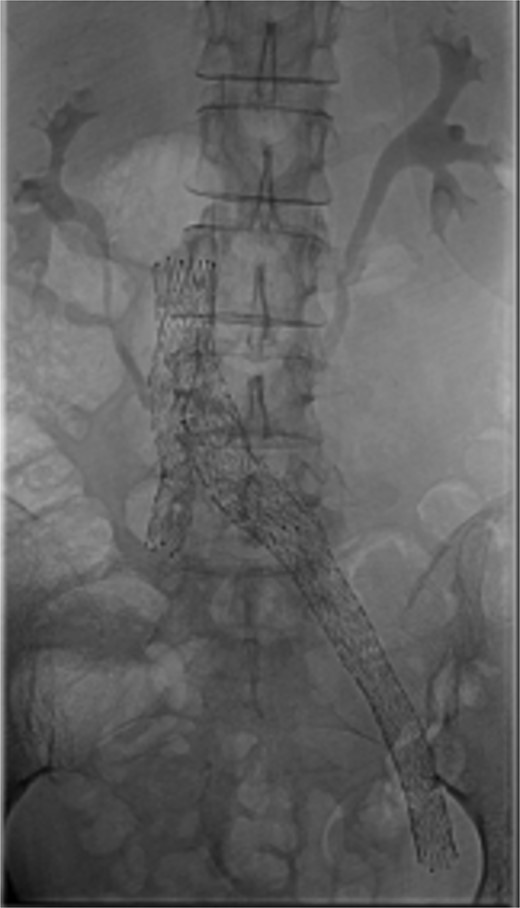
Bilateral popliteal venous access was obtained. Venography confirmed patency of the IVC, left iliac vein, and stents. Thrombolysis of the right lower limb was performed with AngioJet Zelante and 10 mg of alteplase (lower dose to minimize hematoma complications). The IVC filter was then removed to allow extension of a Venovo 12 × 80 mm stent positioned in the right iliac vein, and a Venovo 14 × 80 mm superior extension on the left. Both stents were deployed simultaneously in a ‘kissing’ configuration and post-dilatated with Mustang 12 × 100 mm balloons (Fig. 4). The completion venogram showed smooth contrast flow in both limbs with the disappearance of collateral veins.
The patient had marked reduction in swelling and was discharged home on subcutaneous enoxaparin per the hematologist, with conversion to oral anti-coagulation at outpatient review.
Discussion
PCD is a rare and severe manifestation of acute DVT. Prior pelvic surgery and irradiation predisposed our patient to bilateral iliac vein stenosis and PCD [1, 2].
Thrombolysis options include catheter-directed thrombolysis (CDT), which involves prolonged infusion of thrombolytics and often requires intensive care unit admission, and PMT, which reduces treatment time and thrombolytic dose [3]. AngioJet Zelante uses pulsed sprays to deliver thrombolytics and fragment clots for easier retrieval, followed by rheolytic thrombectomy via high-pressure saline and thrombus aspiration [4, 5]. We chose AngioJet Zelante to achieve rapid clot clearance, with each procedure lasting 2.5–3.5 h and successfully restoring limb perfusion. Alteplase doses used in both procedures were below the average required for CDT as per the PEARL registry [6].
Both CDT and PMT are safer than systemic thrombolysis, requiring lower thrombolytic doses and minimizing systemic drug exposure by direct thrombolytic delivery into the clot [7]. Intracranial bleeding rates following systemic thrombolysis are 3%–6%, compared to up to 1% with CDT [8].
The initial 20 mg alteplase dose was within registry mean and chosen due to extensive clot burden. Unfortunately, the patient still developed a limb-threatening bleeding complication in her hand. This stresses the importance of assessing systemic bleeding risks before thrombolysis. In our second procedure, we learnt that a lower dose of alteplase works as well, suggesting the feasibility of always starting with a lower dose and adjusting based on post-procedural angiographic results.
Following thrombolysis, stenting is often required to address underlying venous stenosis [3]. Although cases of successful bilateral iliac vein stenting have been reported, the initial focus was on saving the symptomatic limb. Given the patient’s narrow caval confluence and collateral drainage of her right lower limb (Fig. 3), we did not deploy ‘kissing’ stents initially.
This case highlights valuable lessons about iliac vein stenting near the caval influence. ‘Kissing’ venous stents are safe, feasible, and should strongly be considered upfront to avoid repeat contralateral procedures. Intra-venous ultrasound (IVUS) has been recommended to guide sizing. It also helps to objectively compare the pre- and post-treatment effects [9]. In our case, IVUS was not available due to the emergency procedures being performed after hours.
If unilateral stenting is chosen, it is important to avoid ‘jailing’ the contralateral iliac vein. This can be achieved, e.g. with the use of a Sinus Obliquus stent (Optimed, Ettlingen, Germany), whose oblique outlet may mitigate the risk of stent struts covering the contralateral iliac vein [10].
Conflict of interest statement
None declared.
Funding
None declared.



