-
PDF
- Split View
-
Views
-
Cite
Cite
Ahmed Almalki, Ahad Alotaibi, Heythem Alzamel, Saud Albuthi, Rare appendicular anomaly of horseshoe appendix diagnosed intra-operatively during laparoscopic appendectomy: case report, Journal of Surgical Case Reports, Volume 2024, Issue 12, December 2024, rjae769, https://doi.org/10.1093/jscr/rjae769
Close - Share Icon Share
Abstract
Acute appendicitis is the most common cause of lower abdominal pain among patients presented to the Emergency Department. Appendicular anomalies in general are rare, and the horseshoe appendix is considered the rarest, with few reported cases in the literature. We are presenting a young female patient, medically and surgically free, who presented to the Emergency Department with persistent right lower quadrant, associated with vomiting for 2 days. Vitally was stable, and labs were remarkable for leukocytosis and neutrophil shift. Abdomen CT scan showed a dilated appendix up to 1 cm with mural edema and hyperenhancement surrounded by mild fat stranding, minimal free fluid, and thickened adjacent peritoneal reflection. In conclusion, routinely performed surgeries can surprise the surgeon with unusual findings. Knowing the anatomy and possible associated anomalies is a cornerstone for any surgery. Even with the rarity of these anomalies, a high index of suspicion and careful recognition are required.
Introduction
Acute appendicitis is the most common cause of lower abdominal pain among patients presented to the Emergency Department with an acute abdomen, and it is the most common diagnosis for young patients admitted to the hospital with acute abdominal pain [1]. Appendicular anomalies in general are rare, and the horseshoe appendix is considered the rarest, with few reported cases in the literature [2–10]. It is a malformation that is usually not discovered in preoperative radiological imaging [2]. The first classification system of the appendiceal anomalies was developed by Cave in 1936, then modified by Wallbridge in 1962, and further modified by Biermann in 1993 [3]. In 2010, a new classification system was proposed by Calota et al., to include the shape in the classification, and the horseshoe appendix was added as it was not defined in any previous classification [4, 5]. The importance of knowing the anatomy, possible related anomalies, and appropriate identifying and classifying these variants is very crucial to the surgeon, as the decision will be made based on them [4]. Moreover, the patient may experience a recurrence of the symptoms due to a missed duplicated appendix that will raise the question of whether an appendectomy was performed or not [4]. Up to date, Jabi et al. summarized all the previous reported cases in their review and found to have a total of 16 published cases globally, the latest reported in Morocco in 2021. This article is reporting the first case of a horseshoe appendix in the Kingdom of Saudi Arabia that was reported previously in the literature.
Case report
We are presenting a 19-year-old, single female patient, medically and surgically free, who presented to Emergency Department with a history of persistent right lower quadrant (RLQ) abdominal pain for 2 days, not improving and increasing in severity, no fever, and no previous similar attacks. On exam, she was stable, no tachycardia, no documented fever, and vital signs upon presentation: blood pressure 116/52 mmHg, heart rate 66 beats per minute, respiratory rate 20 frequency/min, saturating well 100% on room air. The abdomen exam was positive for RLQ tenderness, no rebound, negative Rovsing’s sign, no peritoneal signs. Labs were remarkable for white blood cells: 11.2 × 109/L and neutrophil shift: 8.92 × 109/L, other labs were within normal ranges; pregnancy and urinalysis were negative. Alvarado score was 7. Abdomen computed tomography (CT) scan done (Fig. 1) showed a dilated appendix up to 1 cm with mural edema and hyperenhancement surrounded by mild fat stranding, subcentimeter reactive lymph nodes, minimal free fluid, and thickened adjacent peritoneal reflection. There is no adjacent drainable collection. The unprepared small and large bowel loops are unremarkable. Impression was acute, uncomplicated appendicitis. Patient admitted, prepared for surgery, and laparoscopic appendectomy was planned on the same day of the admission. Intra-operatively, the cecum was identified, which was in the subhepatic area; we followed the taeniae coli; and the appendix was identified in the retrocecal area, and it had two bases, both of which were forming a horseshoe appearance, which is an anomaly of the appendix (Fig. 2). We dissected it off completely till the cecum. Decision made for stapling both bases with an endo-GIA 45 purple. Both bases were stapled. Clean bases were identified, and staple lines were clean, no bleeding, and it was completely healthy. Hemostasis was secured. The patient tolerated the procedure well. The patient was assessed the following day and was doing fine, tolerating orally, passing flatus, with an unremarkable abdominal exam. She was discharged the next day in stable condition. The patient was seen after 2 weeks from the discharge in the clinic and was doing well; clips were removed, and pathology confirmed the diagnosis of acute appendicitis with periappendicitis with a shape anomaly of the horseshoe appendix. Patient planned for colonoscopy in the outpatient department. Interval colonoscopy done that was unremarkable. Patient discharged from the clinic.
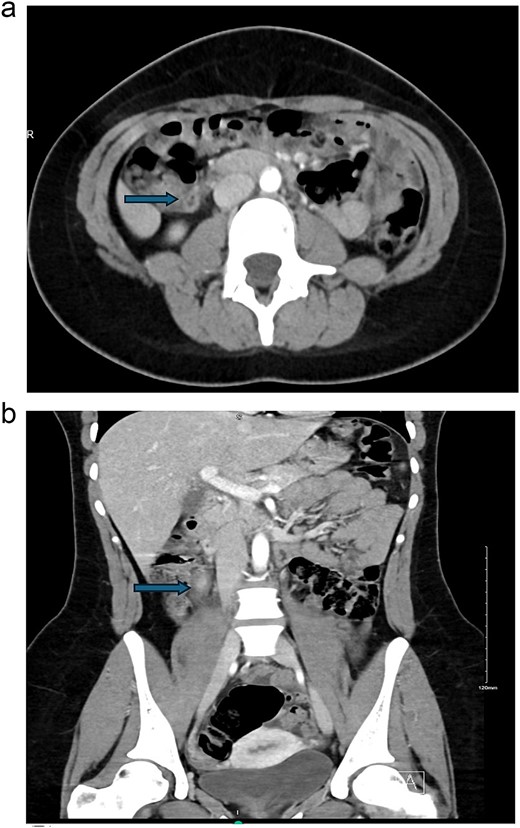
(a) Axial view and (b) coronal view showed a dilated appendix up to 1 cm with mural edema and hyperenhancement surrounded by mild fat stranding, subcentimeter reactive lymph nodes, minimal free fluid, and thickened adjacent peritoneal reflection.
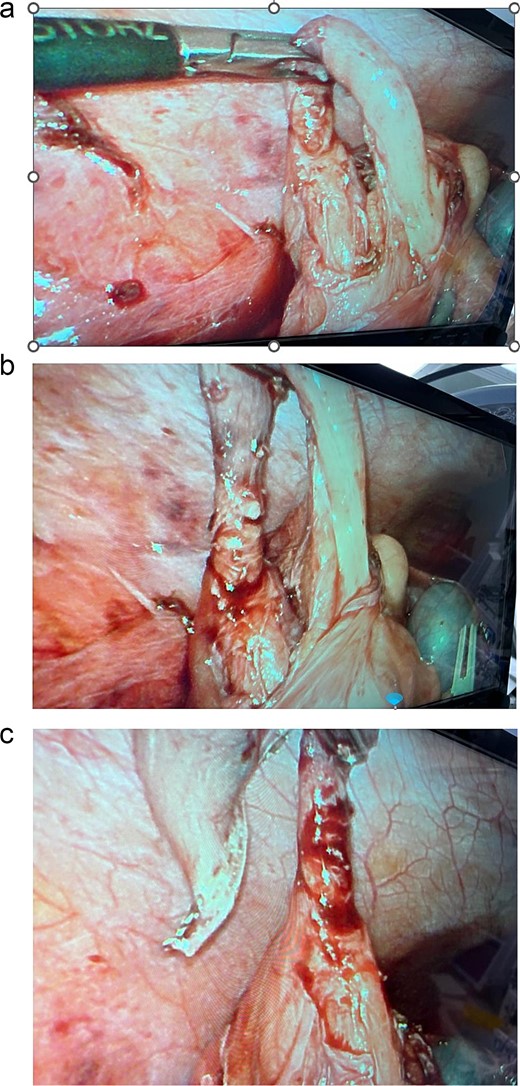
Intra-operative findings of the appendix with two bases connected to the cecum and forming a horseshoe appearance, which is an anomaly of the appendix.
Discussion and conclusion
Horseshoe appendix is a rare entity of appendicular anomaly and rarely reported in literature [4].
Simplified classification system proposed by Calota et al., 2010, to classify the appendicular anomalies based on shape and/or number as shown in Table 1. The numerical appendiceal anomalies were divided to multifarious or congenital agenesis. Multifarious was further categorized based on the duplication, if it was partial or complete. A partial duplication means that both appendices shared a common Y-shaped base on a single cecum (2A), on the other hand, it may have two completely separate appendices, each with its own cecum (2C). Complete duplication of the appendix on a single cecum (2B) was further subcategorized into four types. Lastly, the triplex appendix category (2D), will have a complete triplication of the appendix on the cecum. Regarding shape, the classification mentioned the horseshoe appendix as a shape anomaly with either sagittal or frontal disposal of the mesoappendix [4, 5].
Simplified classification system of appendicular anomalies proposed by Calota et al., 2010 [5]
| Number of anomalies | 1. Congenital agenesis 2. Multiforious appendices: A: appendiceal duplication (partially) in ‘Y-shaped’ B: duplex appendix on a single cecum: with four subtypes: • B1 - ‘avian type’ with intestinal and/or genito-urinary anomalies • B2 - ‘taenia-coli cecum type’ • B3 - ‘taenia-coli hepatic flexure type’ • B4 - ‘taenia-coli splenic flexure type’ C: duplex appendix on a two caeca (each bear an appendix) with hindgut, genitourinary tract, lower vertebral column maldevelopment D: triplex appendix • ‘new-born type’ ± other congenital anomalies; • ‘adult type’whithout other congenital anomalies. |
| Shape of anomalies | • with frontal disposal • with sagital disposal |
| Number of anomalies | 1. Congenital agenesis 2. Multiforious appendices: A: appendiceal duplication (partially) in ‘Y-shaped’ B: duplex appendix on a single cecum: with four subtypes: • B1 - ‘avian type’ with intestinal and/or genito-urinary anomalies • B2 - ‘taenia-coli cecum type’ • B3 - ‘taenia-coli hepatic flexure type’ • B4 - ‘taenia-coli splenic flexure type’ C: duplex appendix on a two caeca (each bear an appendix) with hindgut, genitourinary tract, lower vertebral column maldevelopment D: triplex appendix • ‘new-born type’ ± other congenital anomalies; • ‘adult type’whithout other congenital anomalies. |
| Shape of anomalies | • with frontal disposal • with sagital disposal |
Simplified classification system of appendicular anomalies proposed by Calota et al., 2010 [5]
| Number of anomalies | 1. Congenital agenesis 2. Multiforious appendices: A: appendiceal duplication (partially) in ‘Y-shaped’ B: duplex appendix on a single cecum: with four subtypes: • B1 - ‘avian type’ with intestinal and/or genito-urinary anomalies • B2 - ‘taenia-coli cecum type’ • B3 - ‘taenia-coli hepatic flexure type’ • B4 - ‘taenia-coli splenic flexure type’ C: duplex appendix on a two caeca (each bear an appendix) with hindgut, genitourinary tract, lower vertebral column maldevelopment D: triplex appendix • ‘new-born type’ ± other congenital anomalies; • ‘adult type’whithout other congenital anomalies. |
| Shape of anomalies | • with frontal disposal • with sagital disposal |
| Number of anomalies | 1. Congenital agenesis 2. Multiforious appendices: A: appendiceal duplication (partially) in ‘Y-shaped’ B: duplex appendix on a single cecum: with four subtypes: • B1 - ‘avian type’ with intestinal and/or genito-urinary anomalies • B2 - ‘taenia-coli cecum type’ • B3 - ‘taenia-coli hepatic flexure type’ • B4 - ‘taenia-coli splenic flexure type’ C: duplex appendix on a two caeca (each bear an appendix) with hindgut, genitourinary tract, lower vertebral column maldevelopment D: triplex appendix • ‘new-born type’ ± other congenital anomalies; • ‘adult type’whithout other congenital anomalies. |
| Shape of anomalies | • with frontal disposal • with sagital disposal |
The etiology of the appendicular anomalies remains unclear due to the rarity of the reported cases; however, multiple theories and hypotheses were raised. One of them was assuming that during the embryologic development the base of the appendix may split in two, and during the developmental course, the cecal growth will separate further, leading to a double-based single structure [10]. Yet, no definitive explanation was established.
In conclusion, routinely performed surgeries can surprise the surgeon with unusual findings that may be encountered. Knowing the anatomy and possible associated anomalies is a cornerstone for any surgery. Even with the rarity of these anomalies, a high index of suspicion and careful recognition of any atypical finding are a must.
Author contributions
Authors contributed to the manuscript equally.
Conflict of interest statement
The authors declare that they have no competing interests.
Funding
There was no financial support.
Data availability
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief.



