-
PDF
- Split View
-
Views
-
Cite
Cite
Fayez A Alrohaimi, Nader S Alharbi, Abdulrazaq M Alshammari, Salman K Alotaibi, Resection of accessory parotid gland tumor utilizing trans-oral technique: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 11, November 2024, rjae699, https://doi.org/10.1093/jscr/rjae699
Close - Share Icon Share
Abstract
In this report, we discuss a rare case of pleomorphic adenoma in the accessory parotid gland of a 39-year- old male, which is generally a difficult tumor to manage because of the danger of facial scarring and nerve injury from external incisions. A minimally invasive trans-oral surgical technique was used, resulting in a successful resection without the usual complications, demonstrating a promising option that focuses on cosmetic and functional benefits. The importance of complete preoperative evaluations is emphasized, as is the possibility for broader applicability with additional study, establishing the technique’s efficacy to improve outcomes for patients in similar circumstances.
Introduction
The accessory parotid gland is a salivary gland structure found alongside the major parotid gland in only a minority of the population [1]. Tumors of the accessory parotid gland are extremely rare, accounting for just a small fraction of all salivary gland neoplasms [1]. Pleomorphic adenoma, a benign tumor, is the most common salivary gland neoplasm and can develop in the accessory parotid gland [1].
Historically, surgeons treated parotid neoplasms, including those of the accessory parotid gland, with several forms of parotidectomy, which usually involved external neck incisions [2, 3]. While these treatments are effective, they can cause apparent scarring and facial nerve damage, affecting both the esthetic and physical results [4]. Innovations in surgical procedures have resulted in an increase in minimally invasive procedures, such as the transoral route, which has the potential to minimize some of these consequences [4].
The trans-oral technique for salivary gland surgery offers several advantages over traditional external procedures. Because of the direct access to the gland and the avoidance of dissecting through the surrounding tissues, it reduces the chance of leaving a noticeable scar and avoids the risk of harming the facial nerve [5, 6].
Trans-oral excision of accessory parotid gland tumors remains mainly unexplored, with minimal study on the subject. This is due in part to the condition’s rarity, which causes a lack of widespread knowledge.
Furthermore, choosing suitable patients for this approach necessitates careful attention, as the anatomy and pathology of the presenting tumor may have a considerable impact on the procedure’s feasibility and safety [7, 8].
This case report describes the successfully performed trans-oral excision of a pleomorphic adenoma from the accessory parotid gland. We cover the surgical technique used, intraoperative considerations for the trans-oral approach, and postoperative outcomes. Through this report, we aim to contribute to the growing body of evidence supporting the trans-oral approach to accessory parotid gland tumors and highlight the factors that can guide patient selection and surgical planning.
Case presentation
A 39-year-old man presented for evaluation of a painless, firm right cheek mass that had been growing slowly for the past year. He denied any history of discharge, pain, or numbness. The examination revealed a movable right cheek mass next to the oral commissure, measuring 4 x 3 cm. No overlying skin changes or buccal mucosa changes were noted. The rest of the examination of the head and neck was unremarkable (Fig. 1).

Image showing the mass on the right cheek region (arrow pointed to the mass). The mass was ~4 cm by 3 cm in size, painless, firm, and mobile.
Fine-needle aspiration cytology was performed, and the diagnosis of a pleomorphic adenoma originating from the parotid gland was established.
Computed tomography showed a round tumor under the skin, lateral to the buccinators muscle and anterior edge of the masseter muscle (Fig. 2).
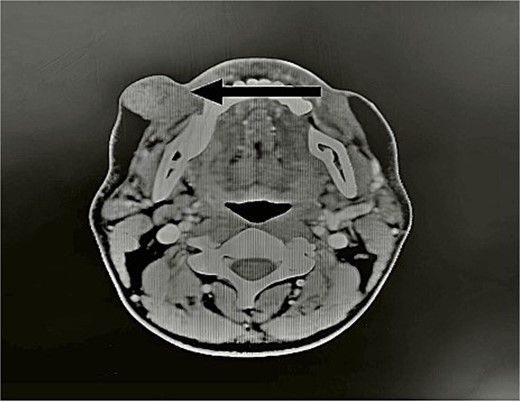
CT scan showed the tumor (arrow). Axial view of head CT scan revealing a mass above the right parotid gland.
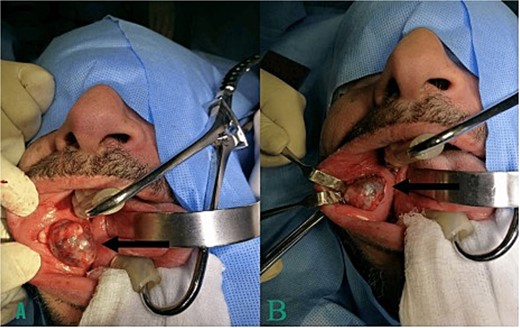
After discussing the complications and benefits of the surgery with the patient, including the possibility of avoiding a scar, he agreed to undergo surgery via a transoral approach (Fig. 3).
The patient outcome was favorable with no postoperative complications over a 9-month follow-up period. The patient did not experience pain, facial numbness, salivary fistula, infection, or cosmetic deformity at the site of excision (Fig. 4).

Patient’s face 2 weeks post-surgery follow-up visit. No visible scar or any facial asymmetry was seen
Discussion
Given their anatomical location and the potential of aesthetics and functional concerns associated with standard surgical techniques, accessory parotid gland tumors present unique therapeutic challenges [4]. The case given herein shows the effective use of a trans-oral approach for the resection of a benign pleomorphic adenoma of the accessory parotid gland, emphasizing numerous significant benefits of this technique.
The trans-oral technique to parotid surgery is not new, but it is less often utilized for accessory parotid gland tumors due to their rarity [9]. The primary advantage of this method is its aesthetic purposes superiority, as it leaves no visible scar, which is of special significance to many patients [6]. In the presented case, the patient was delighted with the outcome, as there was no obvious scarring and the facial aesthetics were preserved.
Functionally, the transoral technique could reduce the possibility of facial nerve damage. The facial nerve is at risk during parotid gland surgery, particularly during the surgical dissection of deep lobe tumors or when the tumor is adjacent to the nerve [10]. The area of incision in our case had been planned carefully to avoid the main trunk and major branches of the facial nerve, which was made more accessible by the direct access offered by the intraoral route. Notably, we did not use nerve monitoring and instead relied on anatomical landmarks and the surgical team’s knowledge. The choice was made based on the tumor’s superficial placement and the low likelihood of nerve entanglement. We were able to properly remove the tumor while keeping the capsule intact, preventing the malignant cells from spreading.
Another essential factor to consider while performing trans-oral resection on parotid tumors is the possibility of developing a salivary fistula or sialocele [11]. However, in this case, no such complications occurred which could be attributed to the wound’s cautious closure and the absence of salivary duct injury during surgery.
The size, position, and proximity of the tumor to the Stensen’s duct must all be carefully considered when selecting patients for a transoral approach. In this case, the tumor’s size and location, anterior to the masseter and lateral to the buccinators, made the intraoral approach feasible [5].
In conclusion, while trans-oral resection of accessory parotid gland tumors is less common than external procedures, it can be a safe and successful option in carefully selected patients. The success of this case, with its positive cosmetic and functional outcomes and lack of severe problems, supports the use of a trans-oral technique in future situations. The ongoing progress in technology that improves the skills and knowledge of head and neck surgeons is expected to lead to an increased range of indications and applications for minimally invasive techniques, such as the trans-oral technique.
Conclusion
We presented a case of a pleomorphic adenoma in the accessory parotid gland successfully excised through a trans-oral approach, highlighting the procedure’s minimal invasiveness and favorable aesthetic and functional outcomes. The technique proved to be a viable option for carefully selected cases, offering a potential alternative to traditional external approaches. Future research is warranted to refine the indications for this technique and to validate its long-term efficacy and safety.
Conflict of interest statement
The authors declare that there is no conflicts of interest.
Funding
No funding was received for this research.
Data availability
The data used to support the findings of this study are available upon request.
Consent
Written consent for publication and patient photography was obtained from the patient.



