-
PDF
- Split View
-
Views
-
Cite
Cite
Konstantinos Tzelepis, Ilias Giannakodimos, Athina A Samara, Christos Kotanidis, Sofia Tsiapakidou, Michel Janho, Antonios Koutras, Sotirios Sotiriou, Complex postoperative ureterovaginal and vesicovaginal fistula following a non-oncological hysterectomy: a report of a challenging complication, Journal of Surgical Case Reports, Volume 2024, Issue 11, November 2024, rjae692, https://doi.org/10.1093/jscr/rjae692
Close - Share Icon Share
Abstract
In a quarter of patients with ureterovaginal fistula (UVF), a concurrent associated vesicovaginal fistula (VVF) can also be found. An increased clinical suspicion should be arised in cases of urinary vaginal discharge accompanied with unilateral flank pain following a gynecological procedure. A 43-year-old female patient diagnosed with a complex postoperative UVF and VVF following a total hysterectomy. After an unsuccessful initial conservative approach with the placement of a nephrostomy tube, an ureterocystotomy with antireflux reimplantation of the ureter was decided. The patient experienced an uneventful postoperative period and a year later, the patient remains asymptomatic without any evidence of fistula recurrent. Our case reports the relatively rare presence of a concurrent postoperative complex UVF and VVF formation in order to rise clinical suspicion in clinicians regarding the diagnostic approach and optimal management.
Introduction
Urogenital fistulas comprise an abnormal connection of the urogenital system with other proximal organs, their incidence not exceeding 2% [1]. The majority of urogenital fistulas are vesicovaginal, while 12%–25% of them involve multiple organs including ureter, bladder, and vagina, with these cases being considered as complex fistulas [1]. Interestingly, in 25% of patients with ureterovaginal fistula (UVF), an associated vesicovaginal fistula (VVF) also coexists, making the burden of the disease more complex and the diagnosis more difficult [1, 2].
The ureter is susceptible to iatrogenic injury during various operations, including vascular, urologic, and gynecologic operations [2]. Injury of the ureter intraoperatively may be a result of either mechanical damage, via ligation and clamping or thermal damage by energy devices such as bipolar [3]. Urinary incontinence, repeated urinary infections, and patient discomfort comprise the most frequently reported symptoms of urogenital fistulas [2]. Cystoscopy, retrograde cystography, nephrotomography, computed tomography (CT), nephrotomography, and cystography are included in the diagnostic armamentarium for the detection of these lesions [2].
Herein, we present the case of a 43-year-old female that developed a complex postoperatively UVF and VVF after a total hysterectomy, emphasize our experience in diagnostic approach and management of a complex disease that impairs patient’s quality of life.
Case report
A 43-year-old female diagnosed with uterine fibroids underwent a total transabdominal hysterectomy due to heave menstrual bleeding. Her medical past history was unremarkable. The postoperative period was uneventful, and she was discharged the fourth postoperative day. However, ten days after the operation, the patient complained for urine discharge from the vagina and right flank pain. Her physical examination confirmed the urinary vaginal discharge, and a positive Giordano sign of the right side was found. An ultrasound examination revealed a mild dilation of the right renal pelvis.
A CT nephrotomography with contrast enhancement was performed and identified an abnormal communication between the right ureter and the vagina reporting an UVF (Fig. 1). Moreover, a retrograde cystography was also performed without any findings. Due to the high suspicion of an intraoperative ureteral trauma, a conservative management was decided and a percutaneous nephrostomy was placed in the right kidney, aiming to prevent further urinary leakage from the vagina and to avoid further dilation of the kidney.
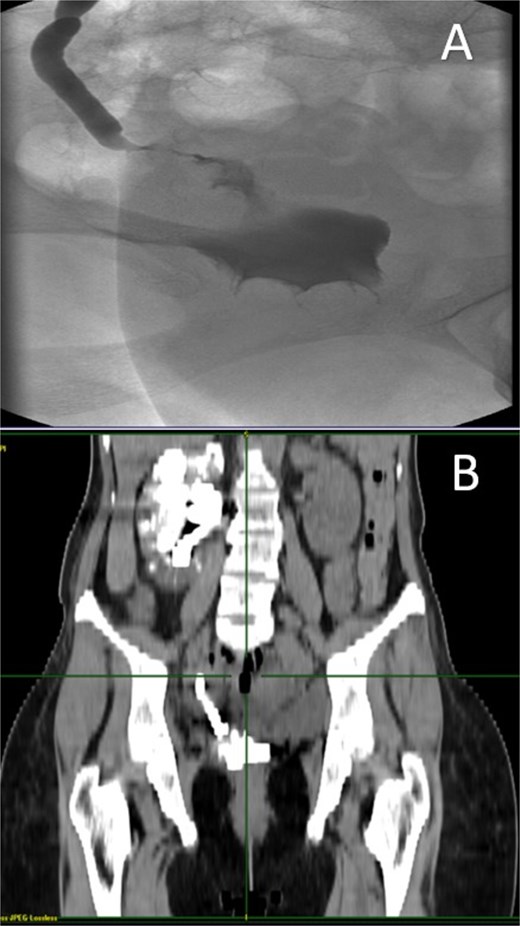
A: Diagnostic nephrotomography showing the existence of an UVF. B: CT nephrotomography showing the abnormal passage of intravenous contrast enhancement fluid from the ureter to vagina, confirming the existence of an UVF.
Two months later, the symptoms gradually reoccurred and a retrograde cystography and CT cystography were performed demonstrating the known UVF and as a new finding the formation of a VVF (Fig. 2). Based on these findings, a surgical repair with an open abdominal exploration was decided.

A: Retrograde cystography with contrast enhancement showing the existence of a VVF. B and C: CT cystography showing passage of contrast enhancement from the bladder to vagina, demonstrating the formation of a VVF.
Intraoperatively, fibrotic adhesions were found and the lower part of right ureter was found clamped with the vaginal stump and bladder and an ureterocystotomy with antireflux ureter reimplantation were performed. Detachment of the ureter from the vagina was performed, using part of the peritoneum to seal the detached area, in order to prevent further fistula formation and the bladder wall was closed in two layers and a transurethral catheter was placed (Fig. 3).
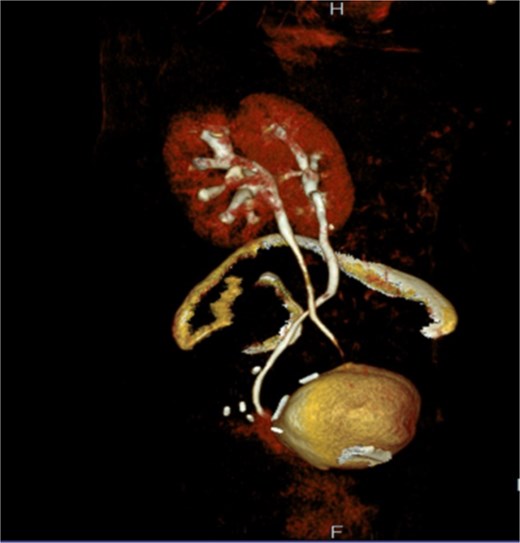
The 3D image of reimplantation of the right ureter with antireflux technique in the dome of the bladder.
The postoperative period was uneventful and the patient was discharged the sixth postoperative day. Transurethral catheter was removed after 2 weeks. In a 12-month follow-up, the patient remains asymptomatic, with no signs of renal dilation in abdominal ultrasound and CT.
Discussion
There is an increased risk of ureteral injuries during gynecological procedures as the gynecological pelvic organs are anatomically proximal to urinary tract [4, 5]. The exact incidence of a postoperative UVF formation following a gynecologic procedure is difficult to be calculated with accuracy, as only symptomatic patients often requiring a surgical intervention are being recorded.
In the developing countries, fistulas occurring during labor are the most frequently reported and are associated with uterine injury at delivery, while in the developed countries, iatrogenic intraoperative injuries are considered as the leading cause [6]. Possible mechanisms for ureter injury and formation of a UVF include injury of the ureter during dissection from the surrounding tissues, clamping or causing thermal injury with energy devices [6]. Sutures or clamping that are located in the ureter can cause pressure and necrosis, tissue loss, and finally a fistula formation [6, 7]. Pelvic adhesions, enlarged uterus, and increased blood loss during surgery comprise main risk factors for the occurrence of UVFs.
Regarding clinical symptoms, postoperative onset of incontinence constitutes the primary symptom of UVFs [8]. Urinary leakage due to incontinence usually start one to four weeks following the operation [9]. During clinical examination, urinary discharge from the vagina is the typical finding in women with UVF, following by urosepsis, infections, and renal failure [10].
The diagnosis of UVF is confirmed by the presence of contrast extravasation from the ureter into the vagina, usually seen in delayed phase in CT scan [8]. In patients with renal failure, MRI with contrast-enhanced T1-weighted or non-contrast T2-weighted image sequences can be useful [11]. Clinicians should be aware that a VVF may coexist with an UVF. Gynecologists should be aware of this rare complication, since early diagnosis is required to prevent further renal damage.
Conservative approach remains the optimal therapeutic management of UVFs, either with the placement of an ureteral stent or with a nephrostomy tube, in order to cease urinary leakage and to avoid renal damage [12]. In cases where a ureteral stent placement is not feasible, surgery with reimplantation of the ureter is required [8]. According to a systematic review regarding the management of UVFs, early stent placement, before 6 weeks, has been associated with better outcomes, while surgery is considered necessary in cases of stent failure, regardless of timing of fistula formation [13]. In our case report, the decision for the performance of ureterocystotomy with antireflux ureter reimplantation was made after initial failure of conservative treatment with nephrostomy tube placement.
Conclusions
In conclusion, complex UVF and VVF are rare postoperative complications of a gynecological operation. Clinicians should be aware of the clinical symptomatology and diagnostic approach, since early recognition is required to avoid further renal damage. Collaboration between gynecologist and urologist is preferred for optimal conservative or surgical management.
Author contributions
Study concept or design: K.T, S.S, I.G; data collection: C.K, M.J, A.K; data analysis or interpretation: A.S, S.T; writing the paper: K.T, I.G, A.S. All authors have revised and confirm the final version.
Conflict of interest statement
Authors have no conflict of interest to declare.
Funding
That study received no funding.
Consent for publication
An informed consent was obtained from the patient for publication.



