-
PDF
- Split View
-
Views
-
Cite
Cite
Utku Kubilay, Huseyin Berk Yaramis, Surgical management of delayed mucosal cyst after rhinoplasty: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 11, November 2024, rjae688, https://doi.org/10.1093/jscr/rjae688
Close - Share Icon Share
Abstract
Mucosal cysts are rare late complications of rhinoplasty, appearing anywhere from weeks to years post-surgery. The cyst’s location can cause both cosmetic and functional issues. Definitive treatment requires complete surgical excision of the cyst and its capsule to prevent recurrence. A 32-year-old man presented with a 2 × 2-cm painless, soft nasal mass 3 years after open rhinoplasty. The mass had gradually enlarged over 6 months, leading to breathing difficulties. Physical examination revealed a pollybeak deformity. Imaging confirmed a well-defined cystic lesion. The cyst was excised through an open rhinoplasty approach, followed by reconstruction using a costal cartilage graft. The postoperative period was uneventful, with no recurrence or issues at 12 months follow-up. We highlight the importance of meticulous surgical techniques in rhinoplasty to reduce mucosal cyst formation. For cysts >1 cm, open rhinoplasty is preferred due to better reconstruction and lower recurrence rates.
Introduction
Rhinoplasty is the most frequently performed type of facial plastic surgery [1]. However, it can be associated with various complications, including mucosal cysts. These cysts can manifest within weeks or years after surgery [2]. In addition to cosmetic concerns, the location of these mucosal cysts can compromise nasal function. Definitive management involves complete excision of each cyst and its capsule to minimize the risk of recurrence [3].
We excised a mucosal cyst from the dorsum using an open rhinoplasty approach during the late stage revision of primary rhinoplasty. The resulting soft tissue defect was reconstructed with costal cartilage.
Case report
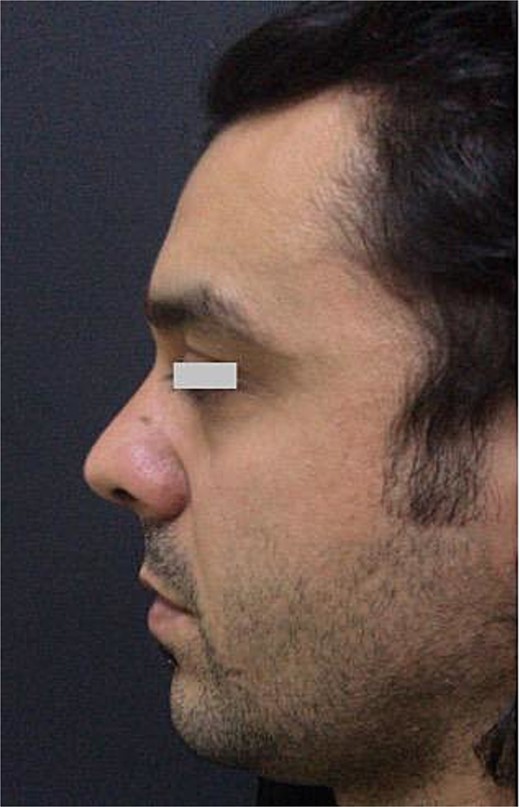
A 32-year-old man with a history of open rhinoplasty 3 years prior presented for the treatment of progressive nasal obstruction that had been present for the preceding 6 months. During the previous 3 months, he developed a painless swelling, gradually increasing, and deformity of the nasal dorsum. In particular, he reported no complications in the immediate postoperative period and had attended regular follow-up for 1 year before discontinuing visits. He denied nasal trauma. Physical examination revealed a soft, non-tender 2 × 2-cm mass on the nasal dorsum, with a characteristic ‘polybeak’ nasal deformity (Fig. 1). Endoscopic evaluation demonstrated a mass that restricts airflow in the bilateral superior nasal valve region, with an intact overlying mucosa. Subsequently, paranasal sinus computed tomography and magnetic resonance imaging were performed (Figs 2 and 3).
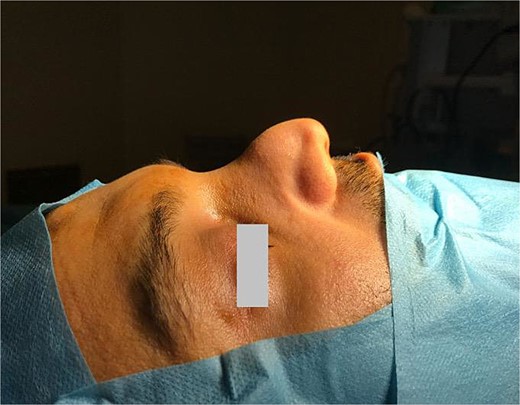
Pollybeak deformity of the nose with dorsal nasal cyst (arrow).

Postoperative computed tomography showing alterations in the nasal dorsum and bone remodeling.

T2-weighted magnetic resonance imaging demonstrating a hyperintense, well defined, 2 × 2 cm lesion in the operative area of the nasal dorsum.
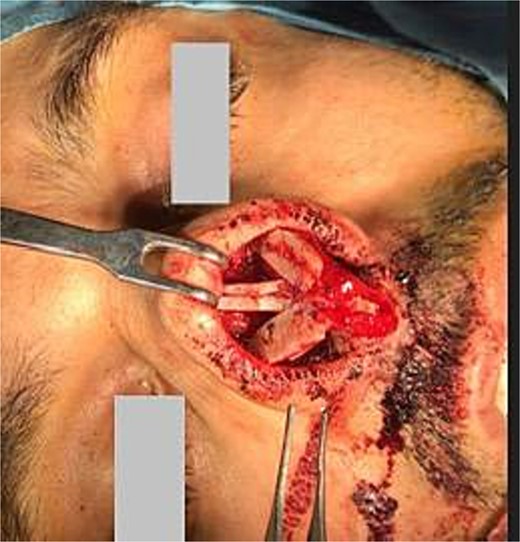
Open rhinoplasty was performed using a Goodman incision and elevation of the skin flap over the alar cartilages, supratip, and nasal dorsum for cyst excision and defect reconstruction with costal cartilage grafts. Dissection revealed a cystic lesion between the upper and lower lateral cartilages, as well as a unique bone attachment measuring ~2 cm × 0.8 cm on the left side (Figs 4 and 5). The cyst and attached bony fragment were excised en bloc to preserve structural integrity (Video S1). In particular, the septum cartilage was not visualized during dissection. A 3 cm costal cartilage graft, harvested from the fifth rib using the oblique split technique, was used to repair the defect. Costal cartilage slices were sutured with 4.0 Prolene as extension grafts to the nasal bone through preexisting turndown holes. Additional costal cartilage slices were interposed inferiorly to create a robust L-strut, then secured using 5.0 Prolene that was passed through a predrilled opening in the exposed nasal spine. Alar cartilages that had been over-resected were reconstructed using costal cartilage grafts. Diced costal cartilage was utilized, mixed with patient’s venous blood, to form a composite graft; This composite graft was wrapped in absorbable oxidized regenerated cellulose (Surgicel, Ethicon, USA) and placed for optimal support. Finally, a cap graft was placed on the tip apex and a strut graft of the alar cartilage was sutured between the medial crura (Figs 6 and 7) The patient reported no functional or aesthetic concerns during the postoperative period.
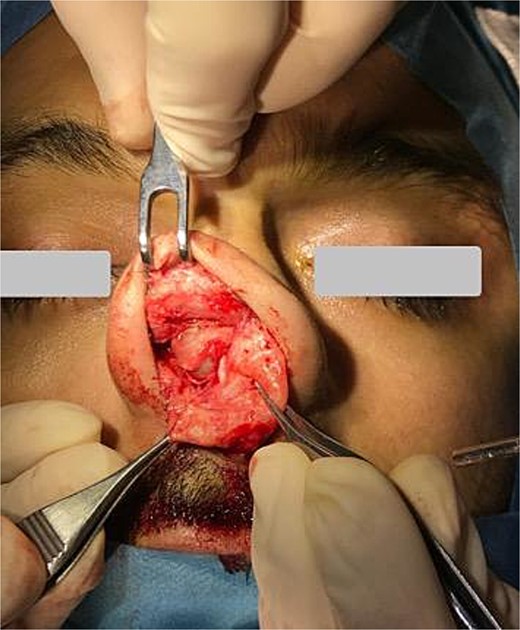
Total excision of the cystic content using an open rhinoplasty approach.
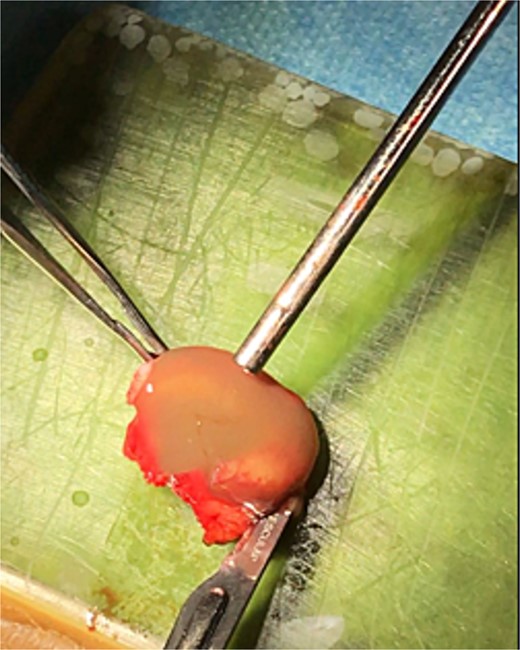
Total excision of the cystic content using an open rhinoplasty approach.
Nasal reconstruction using a costal cartilage graft and postoperative nasal appearance.

Nasal reconstruction using a costal cartilage graft and postoperative nasal appearance.
After surgery, skin sutures were placed; internal Doyle and external thermal splints were applied to stabilize the nasal structure. During the 12-month follow-up period, the patient reported no cosmetic or functional concerns; no signs of cyst recurrence were observed (Fig. 8).
During postoperative follow-up, the nasal appearance was stable without cyst recurrence.
Discussion
Rhinoplasty is associated with a spectrum of postoperative complications, including superficial soft tissue edema, hematoma, lipogranulomas, epidermoid inclusion cysts, proliferation of tumefactive cartilage, mucous cysts, and bone spicules [2]. Mucosal cyst development exhibits a variable timeline, ranging from 5 days to 20 years after surgery [3].
Although the precise mechanisms underlying the development of mucosal cysts remain unclear, three primary theories have been proposed. McGregor et al. [4] suggested that nasal mucosal herniation through the osteotomy line after rhinoplasty contributes to cyst formation. However, this theory has been largely abandoned. Flaherty et al. [5] suggested an association between mucosal damage during osteotomies and cyst development. Mouly et al. [6] proposed that the inclusion of mucosa during grafting procedures could lead to cyst formation. Consistent with the latter theory, we speculate that ectopic mucosal tissue was transferred with the bony graft [7].
Minimization of mucosal trauma during surgery, particularly osteotomies, is crucial to prevent the formation of mucosal cysts [8]. Piezoelectric surgery offers a valuable tool for osteotomies because it reduces internal mucosal injury compared to conventional techniques. Furthermore, meticulous cleaning of harvested bone and cartilage grafts is essential to remove residual mucosa. This process can be facilitated by magnifying loupes or microscopes [9]. More than half of mucosal cysts involve the dorsum. In our case, the cyst remained undetected for 3 years before becoming visible externally. Its inferior growth pattern led to obstruction in both nasal passages, particularly within the valve area [3]. To minimize the risk of recurrence, complete removal of the cyst with preserved integrity is essential. Techniques such as needle puncture aspiration and marsupialization have high rates of recurrence due to incomplete removal [3].
Although various techniques are recommended for the surgical treatment of mucosal cysts, including external closed rhinoplasty, endoscopic, and open rhinoplasty, each has distinct advantages and advantages [10]. External approach, achieved through an incision in the skin, offers a straightforward method of accessing the cyst. However, this method carries a high risk of visible scarring and hinders complete cyst removal, making it a less favorable option for cosmetic procedures (e.g. rhinoplasty). The closed technique requires widening the dissection area within the nose to visualize the cyst. However, achieving sufficient exposure and maintaining control over cyst margins during removal can be challenging, leading to increased risk of recurrence [10, 11].
Endoscopic techniques offer a minimally invasive approach to the management of small mucosal cysts, thereby maintaining cyst integrity. The greatest advantages of endoscopy include the absence of external incisions and minimal dissection, leading to faster healing times [7]. On the contrary, the open rhinoplasty approach, which uses a columellar incision and extensive dissection to reach the cyst, presents considerable limitations [10]; this technique can be utilized for larger cysts (> 1 cm) to facilitate complete excision and mucosal reconstruction, thus minimizing recurrence rates. Mucosal cysts, a late complication of rhinoplasty, can affect functional and aesthetic outcomes. To mitigate this risk, atraumatic osteotomies that preserve the nasal mucosa are crucial. Additionally, meticulous cleaning of harvested bone and cartilage grafts, aided by magnification, is essential to remove residual mucosa [10]. Although endonasal endoscopic total excision is recommended for small mucosal cysts, open rhinoplasty is preferred for cysts >1 cm due to its advantages in reconstruction and lower recurrence rates [8].
Conflict of interest statement
None declared.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
3.



