-
PDF
- Split View
-
Views
-
Cite
Cite
Emily Leung, Andrew Finlayson, A novel, double Limberg flap repair for recurrent pilonidal sinus disease, Journal of Surgical Case Reports, Volume 2024, Issue 11, November 2024, rjae683, https://doi.org/10.1093/jscr/rjae683
Close - Share Icon Share
Abstract
Pilonidal sinuses are chronic inflammation and/or infection of the intergluteal region. Recurrent disease is common and is a source of significant morbidity for affected patients. We present a case of an eighteen-year-old male with extensive recurrent pilonidal disease. A novel technique of a double Limberg flap repair was used, with the vertical axes of each flap positioned to optimise wound tension. The cranio-caudal length of the disease in the natal cleft would have resulted in a large amount of excised normal tissue laterally if a single Limberg flap was considered. To avoid this, we used two Limberg flaps over the craniocaudal length to minimise the laterally excised tissue. The patient made an uneventful recovery with no recurrence at 3 months follow-up. This technique demonstrates the flexibility of the Limberg flap, and that a double flap may be successfully used in extensive disease.
Introduction
Recurrent pilonidal sinus disease is common and is a source of significant morbidity for affected patients. Our case presented with extensive recurrent pilonidal disease. This technique demonstrates the successful use of a double Limberg flap, with vertical axes positioned to optimise wound tension.
Case report
An 18-year-old male presented to colorectal outpatients clinic with a recurrent pilonidal sinus. This is on a background of multiple previous procedures, including incision and drainage of abscess one year prior, and elective Karydakis repair 4 months later with subsequent wound breakdown requiring vacuum assisted closure (VAC) dressing. He has G6PD deficiency, no other chronic conditions, and no remarkable family history.
On clinical examination there were multiple pits over a 10 cm length of midline natal cleft. There were no lateral sinus tracts and no underlying abscess.
The surgeon’s preference for pilonidal sinus is a Limberg rotational flap. However, the cranio-caudal length of the disease in the natal cleft would have resulted in a large amount of excised normal tissue laterally if a single Limberg flap was considered. The decision was made to use two Limberg flaps over the craniocaudal length to minimise the laterally excised tissue.
Technique
The patient was positioned prone. Two oblique, inferiorly based Limberg flaps were marked along the length of the previous Karydakis wound with flaps from opposing sides. The rhomboids were vertically adjacent, however the lower flap was rotated oblique to ensure the most caudal wound was positioned off-centre. Both rhomboids had sides of 40 mm. The angles of the oblique vertical axes were drawn to optimise wound tension (Fig. 1). Each rhomboid had a vertical axis of 55 mm (resulting in a combined vertical axis of excision 110 mm) and horizontal axis of 30 mm.
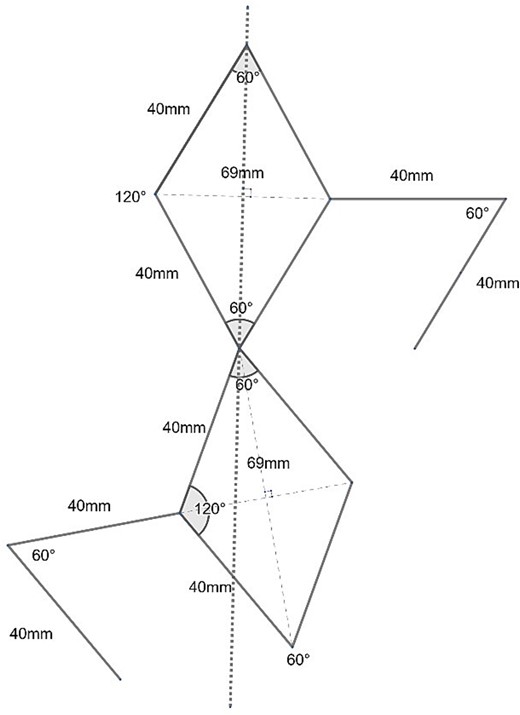
Diagram of position and dimensions of the double Limberg flap. Dotted line – midline; solid lines – incisions.
All sinus tracts were excised. The flaps were rotated into place, a 10-French Blakes drain inserted, and were sutured in three layers with 0 vicryl, 2/0 vicryl, and 3/0 nylon vertical mattress sutures to the skin. Local anaesthetic (Marcaine with adrenaline) was administered.
He made an uneventful recovery post-operatively. Figure 2 demonstrates the scar. Skin sutures were removed after two weeks. He was followed up in the colorectal outpatients clinic for 3 months with no recurrence.
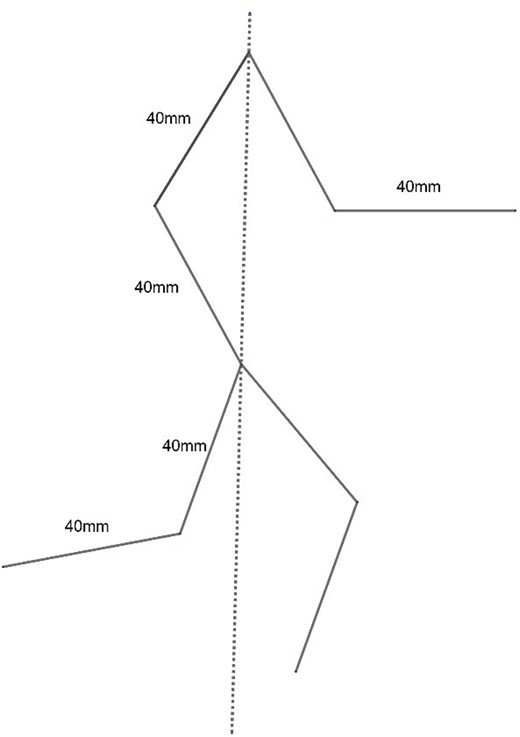
Position and dimensions of scar. Dotted line – midline; solid lines – scar.
Discussion and review of the literature
Pilonidal sinuses are chronic inflammation and/or infection of the intergluteal region. The aetiology is poorly understood, but is thought to be multifactorial, related to a deep natal cleft, penetration of hair shafts through the skin, increased sweat production, and bacterial contamination [1]. The incidence in the general population is 26/1 00 000; mean age at presentation is 19–21 years, with males affected twice as often as females [2].
Management can be complex with frequent complications, such as wound failure, infection, and cyst recurrence [3]. Multiple treatment options exist, ranging from conservative to surgical. The most common are primary open procedures, primary midline closure, Karydakis/Bascom cleft lifts, and Limberg/Dufourmentel flaps [4]. Recurrence rates are variable according to procedure.
A comprehensive meta-analysis by Stauffer et al. [4], including 89 583 patients in 740 studies from 1833–2017, compared recurrence rates for surgical management of pilonidal sinus disease. Across all studies (randomised controlled trials (RCT) and non-RCTs), recurrence was highest in primary midline closure (32% at 120 months; 95% CI 29.6–34.4%), and lowest in the Karydakis/Bascom techniques (2.7% at 120 months; 95% CI 2.4–3.1%). Recurrence for Limberg and Dufourmentel flaps was 11.4% at 120 months (95% CI 9.2–13.7%). When comparing RCTs, however, Limberg and Karydakis techniques had similar recurrence rates, of 1.8% and 2.4% at 24 months, respectively. A systematic review and meta-analysis by Gavriilidis et al. [5] focussing only on more recent RCTs (1999–2019) compared the Karydakis and Limberg techniques and found there to be no statistically significant difference between the two in terms of infection, wound failure, or recurrence.
The American Society of Colon and Rectal Surgeons recommend flap-based procedures for complex or recurrent pilonidal sinus disease [6]. The Limberg flap was described by Limberg in 1946 [7] and has been modified in the management of pilonidal sinus disease, for example, by being positioned with the vertical axis displaced horizontally from the midline, or by positioning the vertical axis oblique to the midline [8].
To our knowledge, there is only one previous report in the literature of two adjacent Limberg flaps sharing a common vertex. Naveen et al. [9] described using two tandem rhomboid flaps for the treatment of recurrent pilonidal sinus disease. Two rhomboid flaps were used to excise sinuses that were 17 cm apart. They report using this technique in 5 patients, with no recurrence in follow-up from 6–18 months. They advocate for the use of two flaps in patients with large sinus tracts. Their flaps, however, were both positioned in the midline, with all vertical apices lying on this midline. We feel it is important to position the most caudal aspect of the wound off the midline as this point tends to have the highest rate of wound breakdown. In our experience positioning the caudal extent of the wound laterally reduces wound complication rates.
One other case of a double rhomboid flap has been reported [10]; in this case, however, El-Tawil et al. positioned the two rhomboids such that they shared a side, rather than just a vertex. The midline passed through the centre of the sides of the rhomboids, rather than through the apices as in Naveen et al. [9]. This approach, with a shared side, results in one of the suture lines being created from two flap edges. In Naveen et al.’s approach, each flap edge is sutured to a fixed edge of the wound.
Our case differed from Naveen et al.’s approach by positioning the vertical axes oblique to, rather than on, the midline. This decision was in order to reduce wound tension and therefore to reduce the chance of wound failure.
Our case demonstrates the usefulness of the flexibility of the Limberg technique, such as using a double Limberg flap for treatment of more extensive pilonidal sinus disease.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
None declared.



