-
PDF
- Split View
-
Views
-
Cite
Cite
Motaz A Selim, Ashley Krepline, Calvin Eriksen, Patrick Murphy, Matthew Cooper, The transplant ureter causing small bowel obstruction following intraperitoneal kidney transplantation: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 4, April 2023, rjad218, https://doi.org/10.1093/jscr/rjad218
Close - Share Icon Share
Abstract
Internal bowel herniation under the ureter of an intraperitoneally transplanted kidney is a rare complication yet carries a high burden of morbidity and potential mortality if not recognized and managed appropriately. We describe a case where early intervention salvaged the bowel without ureteral injury. We also describe a technique to close the space beneath the ureter to prevent further episodes of internal herniation.
INTRODUCTION
Internal bowel herniation under the ureter of an intraperitoneal kidney transplantation is a rare cause of small bowel obstruction (SBO). Two previous cases were reported where bowel strangulation was evident on exploration leading to resection of a segment of the bowel [1, 2]. In one of those cases the ureter was unknowingly divided as it was mistaken for an adhesive band resulting in urinary peritonitis [2]. No published literature describes techniques to obliterate the sub-ureteric space during intraperitoneal kidney transplantation to avoid possible internal herniation. Here we describe a case where early intervention helped salvage the bowel without ureter injury. We also describe a technique to close the sub-ureteric space to prevent further episodes of internal herniation.
CASE PRESENTATION
A 73 year-old man with history of end-stage renal disease secondary to reflux uropathy underwent living donor renal transplantation 23 years prior. The transplant was performed via a right Gibson incision. Review of the medical records indicated the kidney was placed intraperitoneal as the peritoneum was adherent to the abdominal wall from prior right native nephrectomy. The patient underwent multiple subsequent surgeries: right inguinal hernia repair, sigmoidectomy with diverting loop ileostomy and ileostomy reversal. A previous bout of SBO was managed conservatively and resolved with nasogastric tube decompression and intravenous hydration. He presented to the emergency department with signs and symptoms of SBO. Laboratory values were normal except for creatinine of 1.7 mg/dL from a baseline of ˂1.0 mg/dL. A non-contrast computed tomography (CT) demonstrated closed loop SBO and new hydronephrosis of his transplanted kidney (Fig. 1). A nasogastric tube was placed, and the patient was taken to the operating room where multiple non-obstructive adhesions were noted on diagnostic laparoscopy. A congested loop of small bowel was found herniated under the intraperitoneal transplanted ureter causing the ‘double obstruction’ of the bowel and the ureter. Laparoscopic reduction of the loop was unsuccessful thus a laparotomy was undertaken. The bowel loop was reduced, and viability was confirmed clinically and via administration of indocyanine green dye. No resection was required.
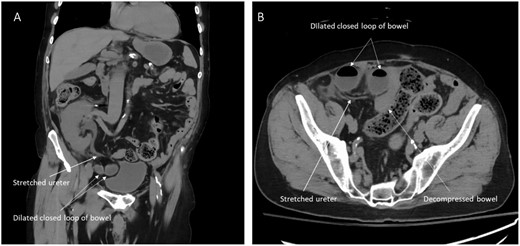
CT images showing herniated ileal loops under the transplanted ureter. (A) Coronal view. (B) Axial view.
The transplanted ureter and the bladder appeared healthy. The bladder was then fashioned over both sides of the ureter (Fig. 2) to obliterate the sub-ureteric space and prevent recurrent internal herniation. The dome of the bladder anterior to the ureterocystostomy was dissected and advanced toward the lower pole of the transplanted kidney in a fashion similar to a psoas hitch. The original ureterocystostomy was maintained in its normal position maintaining its integrity and assuring a lack of tension or compression by the draping bladder. A stent was not felt necessary. Interrupted 4/0 Polydioxanone (PDS® II, Ethicon US, LLC) tacking sutures were used to tack the bladder to the posterior peritoneum overlying the psoas muscle.
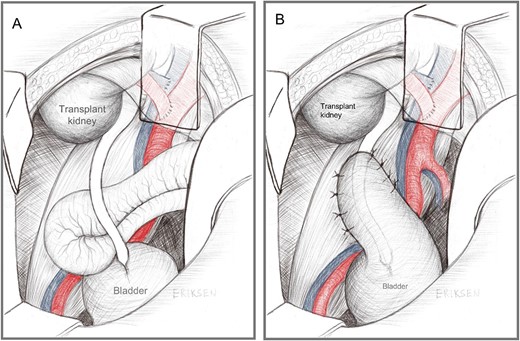
Diagrammatic representation of (A) Herniation of small bowel behind the ‘criminal band’ transplanted ureter, and (B) the modified psoas hitch of the anterior bladder wall to obliterate the sub-ureteric space.
The post-operative course was unremarkable with prompt return of bowel function and normalization of the creatinine level (0.8 mg/dL) at the time of discharge on post-operative day 3. The creatinine level remained stable and there were no surgical complications in the 2 months of follow-up.
DISCUSSION
SBO is a common surgical emergency, resulting in over 300 000 admissions annually in the United States [3]. Adhesions from prior abdominal operations are the leading cause of SBO, accounting for 85% of cases [4]. SBO following kidney transplantation is rare, with a reported incidence of 0.28% in a retrospective review of 1038 kidney transplants [5]. Most kidney transplants are performed using an extraperitoneal approach, this allows for positioning the allograft low in the pelvis and trimming ureteral length to minimize distal ischemia resulting in ureteral stricture. The intraperitoneal space is preferentially utilized in cases of small-sized pediatric recipients, [6] simultaneous kidney and pancreas transplantation and, to a lesser extent, in certain cases following an extraperitoneal approach followed by an elective opening of the peritoneum due to loss of domain or concerns for vascular compromise of the allograft. The intraperitoneal approach is associated with a higher incidence of post-operative gastrointestinal complications including SBO [7].
Two published cases [1, 2] describe SBO due to internal bowel herniation under the sub-ureteric space of an intraperitoneal kidney transplant causing both bowel and ureteric obstruction (dubbed double obstruction) leading to acute kidney injury. In both cases delay in intervention on the closed loop obstruction led to eventual bowel strangulation and resection. One describes further morbidity in which the transplant ureter was mistaken for an adhesive band and unknowingly transected leading to urinary peritonitis and return to the operating room within 48 h for definitive management where the remnant of the ureter was reimplanted into the bladder with the formation of a Boari flap [2]. The second case [1] described revision of the ureterocystostomy without expanding on the indication of the revision. Neither case described a surgical technique to obliterate the sub-ureteric space to prevent further complications.
In the current patient following reduction of the herniated bowel, the ureter was examined and deemed viable and of adequate length. It was felt crucial to close the sub-ureteric space to prevent recurrence of internal herniation and SBO. It was imperative to complete without compromising the vascularity or integrity of the ureter thereby avoiding further obstruction. Revision of the ureteroneocystostomy was thought unnecessary. Recreating the retroperitoneal space with a peritoneal flap would have resulted in tension and kinking of the ureter. As the wall of the urinary bladder was healthy and pliable to easily reach to the lower pole of the transplanted kidney while maintaining the position of the ureter without causing kinks, we elected to use the bladder itself to obliterate the sub-ureteric space in the above described ‘modified psoas hitch’ fashion.
This technique may not be available for every recipient of an intraperitoneal kidney. Thus, we advocate for ongoing discussion regarding additional potential techniques to manage the sub-ureteric space in similar scenarios. This review also seeks to elevate the level of awareness of this rare cause of SBO in patients following an intraperitoneal kidney transplantation. Early recognition and management may salvage the bowel and prevent ureteral injury thus protecting immunosuppressed transplant recipients from major morbidity and potential mortality.
CONFLICT OF INTEREST STATEMENT
All authors deny any conflict of interest.
FUNDING
None.
DATA AVAILABILITY
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Author notes
M.A. Selim and A. Krepline contributed equally to this work.



