-
PDF
- Split View
-
Views
-
Cite
Cite
Shangzhen Geng, Ming Li, Guanghao Chen, Wenqiang Qi, Jianyong Yu, Shu Chen, Hui Meng, Xuewen Jiang, Benkang Shi, Robot-assisted laparoscopic pyeloplasty in an adult with pelvic ectopic kidney with hydronephrosis: a case report and literature review, Journal of Surgical Case Reports, Volume 2023, Issue 4, April 2023, rjad190, https://doi.org/10.1093/jscr/rjad190
Close - Share Icon Share
Abstract
Pelvic ectopic kidney is a congenital anomaly with a higher probability of hydronephrosis than a normal kidney. Few studies have reported cases of pelvic ectopic kidney with hydronephrosis in adults treated with robot-assisted laparoscopic pyeloplasty (RALP). We performed RALP on a 22-year-old male and he recovered well after the procedure. The patient’s pain disappeared after surgery. No complications occurred during the perioperative period and had a rapid postoperative recovery.
INTRODUCTION
An ectopic kidney is a kidney that fails to rise, rises excessively or mistakenly rises to the opposite side due to an abnormal origin of the renal vessels, and its incidence ranges from 1/500 to 1/1200. And pelvic ectopic kidney is one of the most common types of ectopic kidney, with an incidence of 1/2200 to 1/3000 [1]. Ectopic kidneys are more prone to develop diseases than normal kidneys, for example: renal dysplasia, hydronephrosis, kidney stones and infections [2, 3]. Although open pyeloplasty and laparoscopic pyeloplasty (LP) have shown good benefits, these are technically challenging. Therefore, we performed a robotic-assisted laparoscopic pyeloplasty (RALP) in an adult patient with a pelvic ectopic kidney with hydronephrosis.
CASE REPORT
A 22-year-old male admitted to hospital complaining of left lower abdominal pain. Ultrasound and retrograde urography revealed a left ectopic kidney with hydronephrosis (Fig. 1D). Computed tomography angiography (CTA) revealed the left kidney is located in the pelvis with the hilum facing anteriorly; the blood supply from the right common iliac artery and the inferior mesenteric artery and the renal pelvis is markedly dilated (Fig. 1A–C). To check the function of both kidneys, the patient underwent emission computed tomography: glomerular filtration rate (GFR) of the left kidney is 8.88 ml/min and the right is 49.45 ml/min. However, considering the thickness of the left renal cortex on CTA, the impaired function may be due to ureteropelvic junction obstruction (UPJO).

Preoperative imaging findings of the patient. (A) CTA: the left kidney is located in the pelvis with the hilum facing anteriorly; (B and C) the blood supply from the right common iliac artery (the red arrows) and the inferior mesenteric artery (the green arrow); (D) retrograde urography revealed a left ectopic kidney with hydronephrosis.
After communicating with the patient, we performed a RALP. The surgery used a transabdominal approach, and an ectopic kidney was seen on the right side of the lower abdomen with a markedly dilated hydronephrosis. A fibrous strip was removed from the pelvic ureteral junction, and a 5 Fr double ‘J’ catheter was put directly into the ureter (Fig. 2E–G). The operation took 175 min. Postoperative pathological findings are irregular proliferation of surrounding fibrous and smooth muscle tissue (Fig. 2H). The patient’s pain disappeared after surgery. No complications occurred such as urinary leakage or urinary tract infection during the perioperative period. The patient was discharged from hospital 3 days after the surgery. Double ‘J’ catheter was removed 6 weeks after surgery. The blood of urea nitrogen was 4.30 mmol/L, the serum creatinine was 92 μmol/L and the GFR was 101.350 ml/min 3 months after the surgery. CT showed significant reduction in hydronephrosis (Fig. 3I and J).
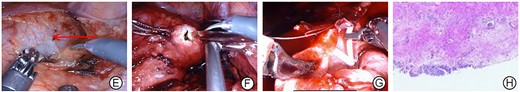
Intraoperative images and postoperative pathology of the patient. (E) Significant hydronephrosis with dilated renal pelvis (the red arrow); (F) the dilated renal pelvis is incised;(G) sutured renal pelvis after the placement of double J ureteral catheter; (H) pathology is an irregular proliferation of surrounding fibrous and smooth muscle tissue.
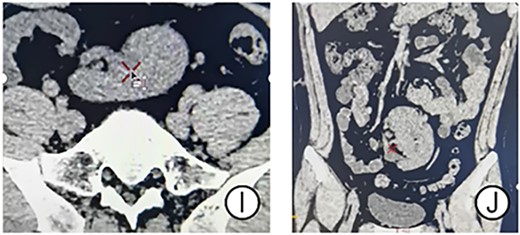
CT results of the patient’s postoperative follow-up. (I and J) CT showed significant disappearance of the effusion.
DISCUSSION
The kidneys originate in the pelvis. During the 6th–9th weeks of embryonic development, the kidney begins to rise to the lumbar. The long axis rotates medially and the renal artery establishes contact with the aorta [1]. As the kidney rises, the vessels supplying it are derived from successive transient aortic branches [1]. The rise of the kidney is restricted when the blood vessels are not fully degenerated. The renal pelvis is often located anterior to the kidney and is accompanied by tortuous ureteral travel. This leads to the development of hydronephrosis, kidney stones and infection [4].
For the diagnosis of ectopic kidney with hydronephrosis, in addition to clinical manifestations and signs, ultrasound, retrograde urography and CT [5] are also required. Ultrasound can initially screen for ectopic kidneys in the pelvis, CTA can show not only the severity of ectopic hydronephrosis, but also the origin, number and variation of the vascular and retrograde urography can show the location and length of pelvic ureteral obstruction. Banthia et al. found that 22–37% of ectopic kidneys were associated with UPJO [6]. In our case, UPJO, which was caused by irregular proliferation of fibrous and smooth muscle tissue, caused hydronephrosis.
A pelvic ectopic kidney usually has no obvious clinical symptoms. In cases with severe hydronephrosis or pus accumulation, timely surgical treatment is required to improve clinical symptoms and preserve renal function. The pelvic ectopic kidney is more difficult to operate on because of the variant location. Common surgical procedures for the treatment of adult pelvic ectopic kidney with hydronephrosis include open pyeloplasty and LP. Ectopic nephrectomy is performed when the contralateral kidney is functioning normally and the ectopic kidney is lost or very poorly functioning [1].
Compared with open surgery, LP has the advantages of being less invasive and having a good surgical field of view, but it has a longer learning curve and requires a high level of teamwork. The disadvantages of LP increase the challenges for surgeons and limit the widespread use. These challenges have contributed to the development of Robotic surgery. Robotic surgery is now used in many routine urological surgeries, for example: adrenalectomy, pyeloplasty, nephrectomy and radical prostate cancer [7].
RALP has the advantages of three-dimensional (3D) surgical field, tremor filtering and high suturing efficiency. The 3D surgical field of view provides a clear view of the structures of the tissues and organs during surgery. The robotic arm has a tremor filtering effect, eliminating the danger during operations caused by physiological tremors, achieving precise excision and suturing. Rishi et al. believed that the RALP not only has a high success rate in simple UPJO cases, but also shows good results in complex UPJO cases [8]. Lukkanawong et al. have reported that robotic surgery can reduce the total operating time, drain removal time and intraoperative blood loss compared with laparoscopic approaches [9].
RALP is currently gaining recognition among pediatric urologists [10]. A study in children found that the success rates of both RALP and LP were similar, but RALP was superior to LP in terms of operative time, length of hospital days and complication rates [11]. However, there are few studies that have reported the cases of pelvic ectopic kidney with hydronephrosis in adults treated with RALP. In the present case, the patient was treated with RALP and the pain disappeared and the kidney function was restored.
In conclusion, the pelvic ectopic kidney is a congenital anomaly that is often associated with complications such as hydronephrosis and renal calculi. With the report of the case, we believe that RALP offers a safe and effective option with few perioperative complications and rapid postoperative recovery for the treatment of ectopic kidney with hydronephrosis in adults.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This work was supported by the National Natural Science Foundation of China (No. 81970661).
DATA AVAILABILITY
The data that support the findings of this study are available from the corresponding author (MBI) upon reasonable request.



