-
PDF
- Split View
-
Views
-
Cite
Cite
Omar A Paipilla, Gabriel A Molina, Juan F Zavalza, Miriam Gil, Maria L Montero, Richard Fuster, Maria E Hernandez, Marisela A Diaz, Looking in a mirror, laparoscopic gastric sleeve in situs inversus patient: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 7, July 2022, rjac341, https://doi.org/10.1093/jscr/rjac341
Close - Share Icon Share
Abstract
Laparoscopic sleeve gastrectomy has been widely accepted and adopted as a weight loss procedure for obesity. Although technically demanding, it is feasible and can improve patients’ overall health. However, any variation from normal anatomy can be challenging for any surgery, especially bariatric surgery, where a mistake could mean going from a life-saving opportunity to costing the patient’s life. We present the case of an obese patient who sought medical attention and decided on bariatric surgery. During her preoperative evaluation, situs inversus totalis was discovered. After careful planning, the surgical team completed the surgery without complications, and the patient recovered completely.
INTRODUCTION
Laparoscopic bariatric surgery has become one of the most valuable tools for treating obesity [1]. However, it is highly technical and therefore must be performed by highly skilled surgeons [1]. On rare occasions, surgeons will face a patient with altered anatomy, increasing the already high challenges for the surgical team [2, 3]. On these rare occasions, the surgeon and his team must rise to the challenge to provide proper treatment in an unfamiliar environment [3].
We present the case of an obese patient with situs inversus who underwent gastric sleeve (GS) surgery; after adapting the technique to the patient’s anatomy, the surgery was completed without complications.
CASE REPORT
Patient is a 31-year-old female with a past medical history of obesity. She told us that since she was a child, she has had problems with her weight; she has tried multiple diets without success and exercise plans and pills. However, none of the treatments were effective. In the last 2 years, she has felt much more tired and has noticed a lot of difficulties exercising. Therefore she sought medical help and was admitted to our bariatric program. On clinical examination, the patient was obese (BMI > 46). Her blood pressure was normal, and she was otherwise healthy. At the examination, no pathology was found, only decreased heart sounds. She started the program with a multidisciplinary team that included a nutritionist and a psychologist.
Preoperative evaluation revealed dextrocardia and that her gastric bubble was located under the right hemidiaphragm. With these findings, an abdominal computed tomography (CT) scan revealed situs inversus totalis (SIT), a condition of which she was unaware at the time. After adequate nutritional guidance, surgery was decided on this patient with a specific surgical plan for the patient’s unusual condition (Fig. 1A and B).
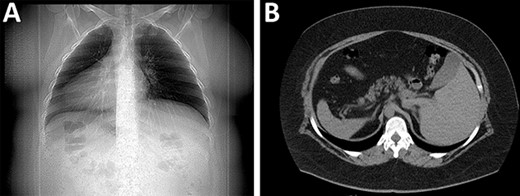
(A) X-rays with the organs in an inverted position. (B) CT revealing the spleen and liver in opposite places.
The patient underwent a GS procedure in the American position. Port site configuration was similar to our conventional GS approach. However, trocar placement was different; we set a 10-mm supraumbilical port for the staples and three 5-mm ports, one on the midclavicular line on the left side of the abdomen, one on the midclavicular line on the right side of the abdomen for the camera and the last 5-mm port on the right anterior axillary line (Fig. 2).

Port positioning of the patient, the camera is on the patient’s right side, and the surgeon is standing on the left.
Before starting the operation, the intra-abdominal cavity was examined and checked for any additional pathology; as it appeared normal, the greater curvature of the stomach was released (starting ~4-cm proximal to the pylorus until reaching the gastroesophageal junction) using an ultrasonic energy device.
As usual, a 36 Fr gastric calibration tube was passed towards the duodenum to give the new formation of the stomach. Endo Staplers were used consecutively for the formation of the GS. The first staple was a 4.1-mm green, and the following four staples were 3.5-mm blue. Following this, a staple-line reinforcement with a non-absorbable suture was completed, the gastric calibration tube was withdrawn, a latex drain was placed and the operation was completed without complications. Operative time took longer than usual, ~130 min (Fig. 3A–C).

(A) Laparoscopy, showing the inverted position of intra-abdominal organs. (B) Stapling done on the stomach. (C) Buttressing suturing over the staple line.
The patient’s postoperative course was uneventful; liquid diet was started 6 h after surgery, and she was discharged on postoperative Day 2. On follow ops, she’s doing ok.
DISCUSSION
In 2022, the World Health Organization (WHO) reported that more than one billion people worldwide are obese, 650 million adults, 340 million adolescents and 39 million children [1]. As this number continues to rise, bariatric surgery has become a valuable option to control this epidemic [1]. However, bariatric surgery and numerous advanced laparoscopic procedures are technically demanding, especially in high-risk patients [2]. Any variation from typical anatomy poses a unique challenge for the surgical team [1, 2].
SIT is an extremely rare congenital abnormality that happens every 1; 5000–20 000 live births, in which there is a mirror image transposition of the abdominal and thoracic organs that change the usual anatomic landmarks entirely [2]. Thankfully is not commonly associated with other cardiopulmonary, digestive and urologic malformations [2, 3]. As our patient experienced.
Aristotle first described this condition in animals, but Fabricius et al. in 1600, first reported it in a human [2–4]. Many variations exist, including situs solitus (normal), situs inversus (reversed) totalis and a spectrum of abnormalities usually called situs ambiguous, characterized by isomerism and heterotaxy in one or more thoracic or abdominal organs [2, 4]. The causes of these variations are not yet fully understood; however, over 100 genes have been linked to laterality defects, including primary ciliary dyskinesia genes [2, 4]. This condition might cause difficulties during diagnostic and therapeutic procedures [2]. Clinically, situs inversus presents no medical disadvantage and is virtually undetectable if the patient is asymptomatic [3, 4]. It can only be suspected after a detailed clinical evaluation (heart sounds) or confirmed during imaging tests [2]. Even so, most gastroenterologists, radiologists and surgeons will never face such a patient [4]. In our case, the situs inversus was detected on the preoperative evaluation, and surgery was planned accordingly.
In laparoscopic procedures, especially in bariatric surgery [4, 5]. The mastery of surgical techniques is essential since possible complications may arise if the technique is not correctly performed [6, 7]. Not only this, the consideration of trocar positioning is necessary as there are no standard port positions in these patients, so the medical team will need to modify these trocars to ensure the principles of laparoscopy triangulation and ergonomy [4, 8]. Laparoscopic bariatric surgery in a patient with SIT is feasible [9]. Since the first case by Wittgrove in 1998, there have been >20 cases in which laparoscopic surgery was achieved [10].
The handedness of the lead surgeon will also affect surgery as most surgical procedures are designed for right-handed surgeons, and situs inversus can pose difficulties when handling the instruments with their left hand [11]. As a result, problems of fatigue can occur, including hyperflex in the trunk, the need to cross hands, and prolonged operative time [5, 6]. Operating time has also been studied, and the average operation time increased by ~50%. This is usually due to the time spent adapting to the altered anatomical situation, as happened in our patient [7].
A combination of medical imaging, teamwork and thorough preoperative evaluation is essential as it can give the fine details of situs anomalies before any surgical treatment. In our case, when SIT was detected, we changed the surgical technique to adapt it to the patient’s condition; although technically more demanding and with a longer operative time, surgery was completed without complications.
CONCLUSIONS
Surgical patients with situs inversus require more creativeness from the surgical team. This case proves that preoperative evaluation is vital in bariatric and all surgical procedures. Also, the surgical technique and the medical team play a crucial role since the procedure will define the patient’s prognosis. Therefore, the need for advanced laparoscopic training for the next generation is critical as these rare cases will demand more from the surgeon and his team.
By sharing our experience of this condition, we hope to guide future surgeons when they encounter these kinds of patients.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



