-
PDF
- Split View
-
Views
-
Cite
Cite
Ali AlImam, Omar AlKhateeb, Acute abdomen in a known case of sigmoid cancer and review of Laplace Law: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 7, July 2022, rjac321, https://doi.org/10.1093/jscr/rjac321
Close - Share Icon Share
Abstract
In this case, we discuss a case of young female patient was admitted with acute abdomen after a week since the diagnosis of a metastatic colon cancer. The case prompts the revision of Laplace Law, which can be grossly proven on the specimen shown below. The patient presented with a peculiar nontender distended acute abdomen, which further explains the pathophysiology of perforation and peritonitis. This case also produces evidence of colorectal cancer present in the younger population allowing more room for investigating other factors causing it.
INTRODUCTION
Cancer has become the leading cause of death as of 2020, accounting of 10 million deaths in 2020 [1]. Cancer death rates have been on the rise since 20th century; a concern that gave rise to the Surveillance, Epidemiology and End Result Program (SEER).
Colorectal cancer (CRC) is one of the most common cancers worldwide. There are many causes and risk factors of CRC. CRC is also present in many inherited diseases. Screening for CRC has increased diagnosis at early stages and aids in the detection of precancerous polyps. Patients with CRC are also at an increased risk of intestinal obstruction due to the intraluminal growth of the tumor. Furthermore, the mass itself can cause microperforations due to the weak cellular connections and the non-muscular nature of the mass, leading to a perforated viscus.
Cancer is the leading cause of death, with CRC accounting for almost 9.4% of cancer-related deaths worldwide [1]. The 5-year relative survival rate for Distant SEER stage in colon cancer is 14%. The lifetime risk for CRC is 4.0–4.3%, and the overall deaths due to CRC are decreasing. However in the younger population (younger than 55) the rates are increasing [2].
CRC has both modifiable and non-modifiable risk factors. The modifiable risk factors include obesity, a sedentary lifestyle, a low-fiber, high-fat consisting of processed red meat diet, alcohol consumption and tobacco smoking. Non-modifiable risk factors include age, inflammatory bowel disease and a family history of CRC or an inherited syndrome (such as Lynch Syndrome, FAP or others…). There are many symptoms in CRC patients, most being chronic such as blood per rectum or hematochezia, changes in bowel habits, anemia and weight loss.
Acute complications include vomiting, obstipation and abdominal distention. CRC-related deaths are most commonly due to the cancer itself and metastasis. However, CRC-induced deaths are decreasing, whereas non-CRC-induced deaths in patients with CRC are on the rise, such as sepsis, COPD and second primary cancers [3].
CASE REPORT
A 41-year-old-female patient was admitted through the emergency department complaining of obstipation for the past couple of days. She is a known case of sigmoid cancer diagnosed by colonoscopy a week prior. The constipation was associated with severe abdominal distention, nausea and dizziness. The patient complained of no vomiting, no fever, no urinary changes, no shortness of breath, no cough, no loss of consciousness and no abdominal pain.
On physical examination, the patient was in discomfort, with unstable vital signs. The patient had a fever of 38–39°C, was tachycardic (133 bpm) and tachypneic (33 breaths per minute). Her blood pressure was stable at 107/64 mmHg.
On general inspection, the patient was out of breath and grunting. The abdomen was distended with the umbilicus midline and in position. There were obvious skin-colored stretch marks in the lower quadrants. On palpation of the abdomen, there was no tenderness, however the abdomen was rigid all over. On percussion, the abdomen was tympanic all over, with no shifting dullness present. On auscultation, there were minimal bowel sounds; <6 in a minute.
The patient was started on antipyretics and fluid therapy. A nasogastric tube was inserted for decompression. A Foley’s catheter was also inserted to measure fluid output and fluid therapy maintenance. The products of the nasogastric tube were 200 ml of intestinal and gastric contents.
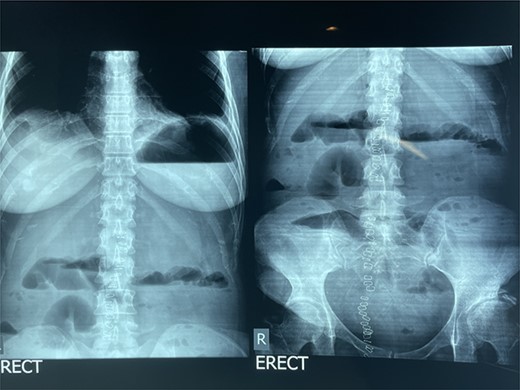
Over the next 24 h, the patient developed obstipation, worsening resistant fever and hypotension (80/42 mmHg). On examination, the abdomen was distended, nontender and rigid all over. The nasogastric tube products were greenish with minimal food content. An erect abdominal X-Ray was ordered, revealing worsening distended bowel with air-fluid levels and air under the diaphragm (see Fig. 1).
The patient’s lab test showed elevated white blood cells preoperatively and decreased white blood cells postoperatively.
The patient was operated on immediately. The surgery was intended as mass excision with perforation repair. During laparotomy, the large bowel was extensively dilated with a gangrenous cecum and ascending colon. No perforation site was found, with microperforations below site of obstruction being the most likely cause for the air under the diaphragm. Thus, a near total colectomy was performed removing 5 cm of the ileum to the distal rectum (see Fig. 2).

Gross image of resected colon revealing gangrenous distended cecum.
During surgery, metastasis to the liver was also evident grossly. An ileostomy was performed in the right lower quadrant, a drain was inserted in the left lower quadrant. The mass was sent for pathology, and the midline incision was subsequently sutured.
DISCUSSION
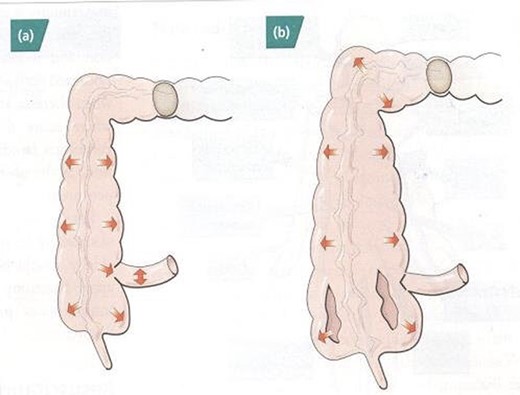
The effect of Laplace’s Law can be clearly appreciated in this case. Laplace’s Law roughly states that, ‘The larger the vessel radius, the larger the wall tension is required to withstand a given internal fluid pressure’. By understanding this, and given the competency of the ileocecal valve (not allowing fluid back-flow into the small intestines); with the cecum being the part of the intestine with the largest radius, we can conclude that the reason for the gangrene and venous insufficiency was due to pressure build up inside the cecum being the highest (see Fig. 3; [4]). However, in this patient, due to rapid intervention, the cecum was saved from being perforated preventing more severe complications.
Early diagnosis and intervention in patients with colonic obstruction is essential to prevent dangerous complications, such as perforation, hemorrhage and septicemia. Evaluation of patients with suspected obstruction is dependent on the clinical findings as well as imaging [5, 6]. Preferably, a CT scan with IV contrast is ordered for clinically stable as it can identify the etiology and any points of transition as well as areas of ischemia or pneumatosis intestinalis suggesting necrosis and perforation. However, if a CT scan is unavailable or is not efficient and is time consuming; an abdominal X-ray is recommended (see Fig. 4).
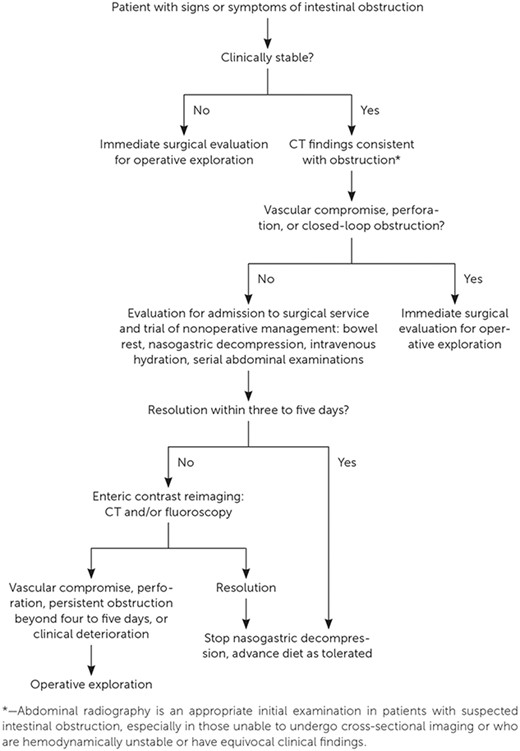
Approach for diagnostic imaging in suspected intestinal obstruction.
In a study performed in 2018 [7], neoplasms were found to be the second major cause of intestinal obstructions after adhesions. Moreover, surgical intervention is recommended in all patients who are clinically deteriorating to prevent complications. In addition, stable patients with known neoplasia are recommended to be treated operatively for palliative decompression and prevention of recurrence in comparison to patients who underwent medical intervention.
CONCLUSION
CRC is a very common and potentially life-threatening disease, which is now being diagnosed in younger patients more often. Clinical suspicion of intestinal obstruction requires urgent diagnosis and intervention to prevent complications. CRC especially in the transverse, descending and sigmoid colon will lead to cecal dilatation as explained by Laplace Law. Clinically unstable patients at any point of hospitalization with high suspicion of obstruction should undergo laparotomy urgently, providing life saving measures.
ACKNOWLEDGMENTS
Dr Ali AlImam and Dr Omar AlKhateeb would like to thank Dr Osama AlSaffarini and Dr Raed Abu Ghosh for their help on this case and their insight into the clinical side of the pathophysiology of colorectal cancer associated intestinal obstruction.
CONFLICT OF INTEREST STATEMENT
In compliance with the ICMJE uniform disclosure form, both authors declared no financial support or relationships were received or formed for this case report. No other relationships were formed or have influenced the reporting of this case.
DISCLOSURE
Case subject: Consent was obtained by the patient and family.



