-
PDF
- Split View
-
Views
-
Cite
Cite
Krishna P Subedi, Shashank Timilsina, Krishna Kumar Yadav, Suraj Shrestha, Prasan B S Kansakar, Jejunojejunal intussusception in an adult due to adenoma: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 7, July 2022, rjac343, https://doi.org/10.1093/jscr/rjac343
Close - Share Icon Share
Abstract
Intussusception is a rare condition in adults and presents a diagnostic challenge. Clinical presentation tends to be chronic and non-specific. Unlike the pediatric population, most adult intussusceptions have structural lesions as lead points. Here, we present a case of jejunojejunal intussusception in a 27-year female due to adenoma of small bowel.
INTRODUCTION
Intussusception can be defined as telescoping of one segment of the gastrointestinal tract into adjacent one. It is a relatively common cause of acute abdomen in the pediatric population. In adults, it is a rare condition that presents as chronic intermittent abdominal pain with features of bowel obstruction [1]. Diagnosis is often delayed as it shares many clinical features with other morbid conditions like appendicitis, pancreatitis, abdominal hernias, colic, volvulus and Meckel diverticulum. Also, classical triad of intussusception (abdominal pain, palpable mass and bloody stool) is rare in adult intussusception [2]. While pediatric intussusception is mostly idiopathic, adult intussusception usually has an identifiable structural abnormality, usually a benign or malignant tumor. In the small intestine, the etiology for intussusception can be inflammatory lesions, Meckel’s diverticulum, postoperative adhesions, lipoma, adenomatous polyp, lymphoma, metastasis or sometimes iatrogenic. Among these, adenomatous polyp is very uncommon [3, 4]. Because of structural abnormalities, most adult intussusception requires operative management [5, 6]. We present a case of jejunojejunal intussusception in a 27-year-old female from a low- and middle-income country.
CASE REPORT
A 27-year-old female presented to the emergency department with a chief complaint of abdominal pain for the past 1 month. Pain was insidious in onset, intermittent and localized to the right hypochondrium. The patient had multiple episodes of non-bilious and non-blood-stained vomiting for the past week. The patient had normal bladder and bowel habits. Review of systems was negative for fever, weight loss, oral ulcers, skin lesions, joint pain or ocular symptoms. The patient did not have any significant past history or family history. The patient was otherwise in good health and was not taking any medications.
On examination, the patient was an average built female in moderate discomfort. She had a temperature of 98°F, pulse of 78 beats/min, blood pressure of 130/70 mm Hg, respiratory rate of 20 breaths/min and oxygen saturation of 97% in room air. General physical examination was unremarkable. Examination of the systems was also unremarkable except for per abdominal examination where tenderness was present over the right hypochondrium. However, the abdomen was soft and there was no palpable mass.
Biochemical and hematological investigations were unremarkable with a total leukocyte count of 8.9 K/μl and a hematocrit of 39.3%. Liver function tests, pancreatic enzymes and electrolytes were within normal range. Plain computed tomography (CT) scan (Fig. 1) of the abdomen revealed ~9.6-cm length long segment invagination of proximal jejunal loop into lumen of immediate distal jejunum. Another similar ~7.7-cm long segment invagination of ileum into lumen of immediate distal ileum was seen. No definitive features of bowel obstruction were seen. There were few enlarged mesenteric lymph nodes seen at the neck of the lesion measuring up to 16 × 11 mm.

Long segment invagination of proximal jejunal loop into lumen of immediate distal jejunum.
Consultation with general surgery was made and the patient was taken to the operation room for exploratory laparotomy. Inspection of the bowel showed a single intussusception at ~160 cm from duodenojejunal (DJ) junction and dilated bowel loops were present at the intussusception site with four polyps (Fig. 2). The intussusception was reduced manually, part of the jejunum with polyps was resected and end to end anastomosis was done in two layers. The histopathology report of resected polyps showed benign lesions (tubulovillous adenoma) (Fig. 3). Postoperative period was uneventful and the patient was in follow-up till 1 year, during which she had been in her usual state of health.

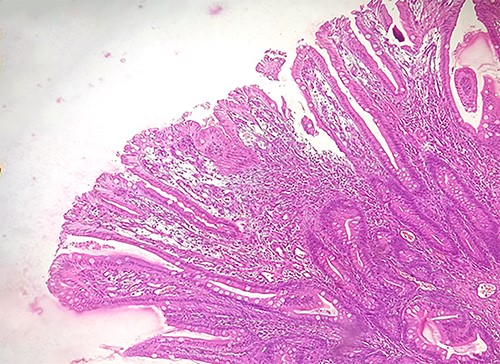
The polypoidal structures from the resected segment of the bowel were lined by intact columnar epithelium and consisted of villi and tubules (tubulovillous adenoma).
DISCUSSION
Intussusception has been classified on the basis of location into entero-enteric (involving small bowel), colo-colic (involving large bowel), ileo-colic (invagination of terminal ileum into ascending colon) and ileocecal (where ileocecal valve acts as leading point) [7]. The vast majority of intussusception in adults is almost always secondary to an identifiable structural cause such as benign or malignant lesions that act as a lead point. The lead point in the small bowel is usually benign lesion, whereas in the colon tends to be malignant [5]. In intussusception, the bowel wall may undergo ischemic necrosis due to compression of vessels in the mesentery that may get trapped between overlapping layers of bowel [6].
Adult intussusception is diagnosed preoperatively in only about 58% of the cases [5]. CT scan and ultrasonography are the main modalities of investigation for diagnosis of adult intussusception [8]. In low- and middle-income countries, diagnosis of intussusception in adults can be delayed, not only because of rarity of the entity but also because of lack of diagnostic facilities [9]. Delay in diagnosis leads to complications like intestinal obstruction, ischemia, perforation and undiagnosed malignancy, which increases morbidity and mortality. Surgical management is the treatment of choice for management of adult intussusception due to higher incidence of structural abnormality [5]. Although controversy exists in the management of adult intussusception, small bowel intussusception can be reduced in cases where benign lesion is identified preoperatively or if there is risk of short bowel syndrome, whereas colonic intussusception should be resected without attempting reduction due higher incidence of malignant lesion as lead point [7, 10]. In our case, polyps were not diagnosed preoperatively and were identified only after thorough inspection of the bowel during laparotomy. During laparotomy, the entirety of bowel should be inspected as there might be features that are not visible in the radiological investigations.
CONCLUSION
Intussusception is a diagnostic challenge due to its unusual presentation in adults. CT scan and ultrasonography are the best investigation tools for early preoperative diagnosis of intussusception. Adult intussusception requires operative management. Clinicians should be aware of the potential for the occurrence of intussusception in adult patients presenting with abdominal pain and features of bowel obstruction.
CONFLICT OF INTEREST STATEMENT
None declared.



