-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammed F Shaheen, Sulaiman Alsugair, Saad M AbuMelha, Mohamad Almarastani, Abdulrahman Altheaby, Salvage of an iatrogenic partial allograft nephrectomy during caesarean section—a case report, Journal of Surgical Case Reports, Volume 2022, Issue 5, May 2022, rjac226, https://doi.org/10.1093/jscr/rjac226
Close - Share Icon Share
Abstract
Since transplanted kidney allografts are standardly placed in a heterotopic pelvic position, any surgical intervention in the pelvis carries the potential risk for allograft injury. A 41-year-old female G4P2 with history of prior kidney transplants presented for an elective cesarean sections (CS). During the CS, profound bleeding was encountered and was later realized to be from the transplanted kidney allograft. A complete transection of the upper pole with the injury extending to the hilar structures was noted. Careful intraoperative evaluation led to the decision favoring a salvage attempt of the remaining part of the allograft. The patient continues to enjoy sufficient allograft function 6 months after the incident. To conclude, although CS after kidney transplantation is considered safe, the risk of allograft injury remains possible with potentially catastrophic consequences. This case highlights the importance of rapid surgical expertise and appropriate preoperative evaluation, preparation and planning.
INTRODUCTION
Kidney transplantation is the preferred treatment modality in patients with end-stage kidney disease in terms of cost-effectiveness, quality of life and survival rate [1]. Under usual circumstances, the transplanted kidney allograft is placed in a heterotopic pelvic position. This leads to the potential risk of allograft injury during surgical interventions in the pelvic area. Urologic surgeries carry the highest potential risk of injuring the allograft [2, 3]. However, allograft injury has been reported with other abdominopelvic surgeries [4–7].
Cesarean sections (CS) is frequently used as a method of delivery post kidney transplantation [8]. Despite the recognizable theoretical risk of injury to the kidney transplant allograft during CS, it appears to be very low [9, 10]. This case report brings to the literature the first significantly consequential allograft injury that occurred during CS with a description of a successful surgical salvage attempt. This study obtained ethical review board approval number (NRC21R-174-04).
CASE REPORT
A 41-year-old female teacher G4P2 post second-time kidney transplantation presented to the hospital for her third elective CS at full term. The patient’s first kidney transplant was performed 19 years prior, in the right iliac fossa. The second kidney transplant was performed 4 years prior, in the left iliac fossa, which continued to function well until her presentation. The later surgery was complicated by a wide-neck incisional hernia containing small bowel loops and fat (Fig. 1). It was left untreated due to lack of symptoms and patient’s hesitation to undergo surgery over the functioning kidney allograft.
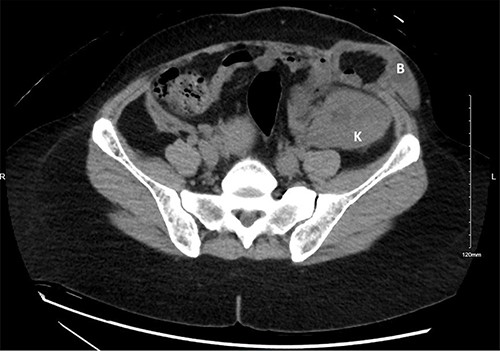
A computed tomography scan of the abdomen with no intravenous contrast obtained 3 years prior to the sentinel event. The kidney allograft (K) appears in the left iliac fossa just beneath a wide-neck abdominal wall incisional hernia with protruding small bowel loops (B).
Under spinal anesthesia, the CS operation was initiated through a Pfannenstiel incision. Upon traction of the recti muscles, unexpected profound bleeding was encountered just below—what was thought to be—the left rectus muscle. Further dissection to optimize visualization resulted in more bleeding. At this point, it was realized that the bleeding source was an injury to the transplanted kidney allograft. Subsequently, the patient was intubated, resuscitated with packed red blood cells and the CS finalized. Urgent intraoperative consultations to the urology and transplant teams were requested.
The urology and transplant teams assessed the injury. The injury to the kidney allograft extended through the upper third of the parenchyma and skived toward the hilum violating the upper polar vessels and calyx (Fig. 2). After bleeding control, assessment of the remaining part of the allograft was performed using intraoperative doppler ultrasound and cystourethrogram (Fig. 3). Doppler ultrasound revealed that most of remnant allograft had an intact arterial signal with exception of a geographical area proximal to the cut edge equivalent—roughly—to 20–30% of the remaining allograft. The venous signal was intact with no concerns (Figs. 2 and 3). The cystoscopy and retrograde pyelography revealed an intact lower calyx. The upper calyx was violated but not vital to the urinary drainage of the remnant allograft. The remnant part of the allograft constituted roughly 65% of the total allograft size. Thus, the decision was made to proceed with a salvage attempt.
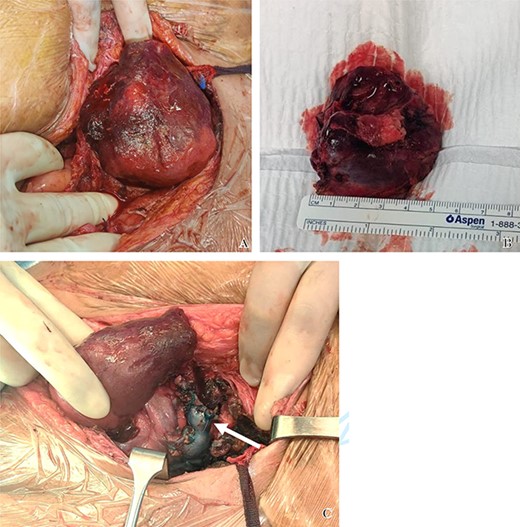
Intraoperative photos. (A) The allograft cut surface after removal of the upper pole. The geographic discoloration reflects presence of areas of poor perfusion is evident. (B) The excised upper pole due to iatrogenic injury. (C) Intraoperative photo of the allograft kidney when medialized. The ligated upper calyx appears stained blue (white arrow) due to testing with the methylene blue to assess for areas of potential leak.
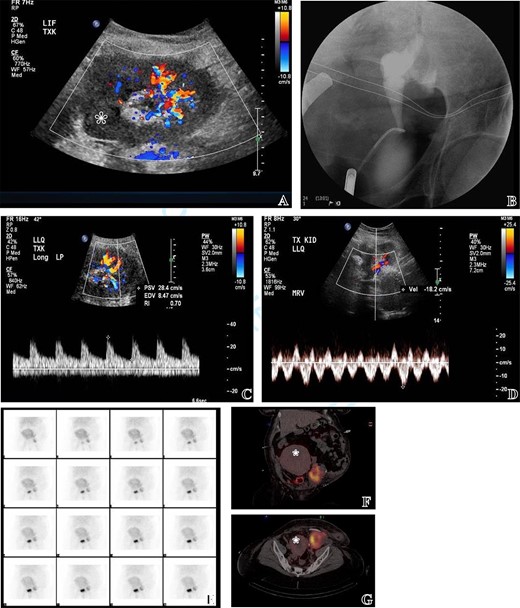
(A) Intraoperative US doppler at the cut surface of the allograft revealing partial perfusion of the allograft as some areas lacked vascular signal reflecting poor perfusion (labelled with asterixis). (B) Intraoperative retrograde ureterogram to test for urine
leaks after closure of the upper calyx. (C, D) Post-operative US evaluation revealing preserved arterial and venous signals in the perfused parts of the allograft. (E, F, G) Post-operative diagnostic MAG3 scan documenting preserved perfusion and function of the allograft with no evidence of leak. The images demonstrate the proximity of the allograft to the gravid uterus (uterus labelled with asterixis).
A Double-J (DJ) stent was inserted followed by the closure of the upper calyx with running polydioxanone suture in two layers. To ensure watertight closure, 250 ml of methylene blue was injected through the Foley catheter and allowed to reflux through the DJ stent. A careful examination of any calyceal openings or bleeding sites requiring closure at the cut surface was done. A perinephric drain was left in place and the wound was closed. After the surgery, the patient was transferred to the intensive care unit for monitoring. Fortunately, renal replacement therapy was not required. Her peak creatinine after the surgery was 553 μmol/l on post-operative Day 5, corresponding to an estimated glomerular filtration rate (eGFR) of 8 ml/min/1.73 m2 (Fig. 4).
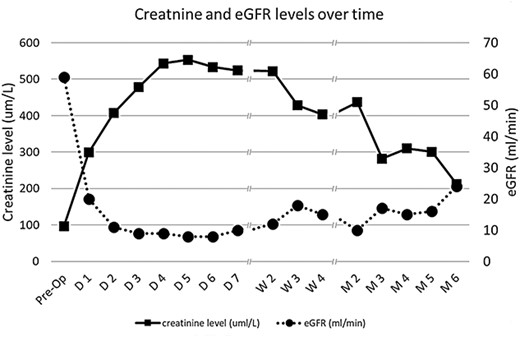
Time lapse of creatinine values and the corresponding eGFR from the immediate preoperative value to 6 months after the cesarean section operation where the iatrogenic allograft injury took place. D (#) = the number of days after the sentinel event; W (#) = the number of weeks after the sentinel event; M (#) = the number of months after the sentinel event.
The post-operative course was complicated by a urinary tract infection with Candida albicans and klebsiella pneumonia. This was managed by antifungal and antimicrobial coverage in combination with a change of the Foley catheter. The patient also required social and psychiatric support due to low mood, anxiety and loss of appetite. The surgical drain and DJ stent were removed on post-operative Days 17 and 22, respectively. The patient was discharged from the hospital after 23 days with a serum creatinine of 322 μmol/l and an eGFR of 15. Six months post-operatively, serum creatinine dropped to 212 μmol/l with corresponding eGFR of 24 ml/min/1.73 m2 (Fig. 4).
DISCUSSION
Placement of the kidney allograft may vary during transplantation surgeries. It is sometimes placed closer to the rectus muscle, which makes it vulnerable to injury if a classic Pfannenstiel incision is planned. In addition, adhesion may make the kidney allograft inseparable from the abdominal wall hindering easy recognition of injury.
Upon literature search, we were able to find only two prior case reports with similar injury patterns during CS. Both had relatively minor allograft injuries with excellent post-operative outcomes [7, 8]. The altered abdominal wall anatomy described in our case, potentially played a role in delayed injury recognition leading to an extensive injury to the allograft before full realization. Luckily, through salvaging the remaining portion of the allograft the patient was spared from the need for dialysis.
This case report stresses the importance of appropriate perioperative evaluation and planning for pregnant ladies with prior kidney transplantation. That is particularly true in patients with complex surgical history. It is certainly advocated to utilize appropriate imaging modalities preoperatively to assess the location and vascularization of the allograft to avoid subsequent injury [2]. In cases where this is not feasible, consideration of a vertical incision during CS may be appropriate.
This case also highlights the importance of early involvement of experts as allograft salvage is possible and can significantly alter the outcome of the patient. The importance of a multidisciplinary team approach before or during the surgery is vital to reach the best possible outcomes.
CONCLUSION
Cesarean section in patients with prior kidney transplantation carries a small, yet significant, risk of kidney allograft iatrogenic injury. Careful organ mapping and planning of the surgical incision to avoid injuries to the allograft is warranted in some cases. Early involvement of multidisciplinary teams is recommended before or during surgery if concerns arise.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



