-
PDF
- Split View
-
Views
-
Cite
Cite
Yi Th’ng Seow, Bindu Kunjuraman, Rare case of gigantic ulcerating phyllodes tumour in developed country with a review of the literature, Journal of Surgical Case Reports, Volume 2021, Issue 3, March 2021, rjab060, https://doi.org/10.1093/jscr/rjab060
Close - Share Icon Share
Abstract
Phyllodes tumour (PT) is a rare type of fibroepithelial breast tumour that can present in a wide spectrum of biological behaviours, accounting for <1% of breast malignancies. Herein, we present a case of a rare gigantic ulcerating PT in a middle-aged woman from regional Western Australia, who presented with a rapidly growing right breast mass. Core biopsy showed spindle cell lesion with differentials being PT of at least borderline variety or metaplastic carcinoma. The ulcerations over the fungating tumour showed heavy growth of Staphylococcus aureus. The treating team subsequently proceeded to right total mastectomy with level 1 and 2 axillary clearance. This report emphasizes the rare presentation of PT, dilemma in investigations and the difficulties in managing non-compliant patient where treatment protocol needs to be modified.
INTRODUCTION
Phyllodes tumour (PT) was originally described by Johannes Muller and was termed as cystosarcoma phyllodes. It is, however, a misnomer as it rarely displaces cystic components and is not a true sarcoma by either cellular origin or biologic behaviour. To avoid confusion, the World Health Organisation officially renamed it as PT [1]. PT usually presents in middle- aged females, with Asian and Hispanic patients more likely to have larger sized tumours (>51–100 mm) compared with their white counterparts [2, 3]. Patients usually present with rapidly growing, mobile and painless breast masses. Given their rarity, it is infrequent to encounter a giant PT. PT often requires further investigations to differentiate between fibroadenoma and soft tissue sarcoma as they have very similar clinical and histological characteristics. The diagnosis for giant breast lumps is crucial preoperatively as it affects operative technique and post-operative follow-up.
CASE REPORT
A 49-year-old lady presented to the emergency department (ED) with features of sepsis on a background of a rapidly growing right breast lump. Patient reported that she first noticed a small breast lump 2 years ago, which was slow growing and progressed significantly larger 4 months ago with overlying skin changes. Initially, her general practitioner referred her to a specialist; however, she was not contactable and only decided to self-present to ED due to pain from the superadded infection on the fungating lesion.
On physical examination, the right breast measured 31 × 23 cm with two well-circumscribed ulcerating wounds over the tumour, which were clinically infected (Fig. 1). On palpation, the right breast was hard and there was palpable ipsilateral axillary lymphadenopathy. The left breast examination was unremarkable.

The right breast mass with two ulcerating wounds at centre, stretched-out erythematous skin.
The wound swab showed heavy growth of Staphylococcus aureus susceptible to Flucloxacillin. On ultrasonography, the right breast was completely replaced by a massive solid, heterogenous mass. It demonstrated internal vascularity and numerous cleft cystic spaces and leaf-like internal architect. Mammogram was not feasible due to the incompressible nature of the right breast, patient discomfort and the size of the lesion. A chest computed tomography was ordered for staging/metastatic workup and preoperative planning. Multiple enlarged right axillary lymph nodes measuring up to 12 mm and a 19 mm lymph node in the right supraclavicular region were noted with no distant metastasis (Fig. 2). The core biopsy showed features of spindle cell lesion with the differentials being borderline PT versus metaplastic carcinoma.
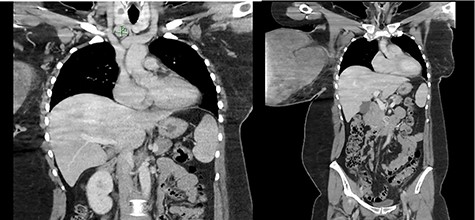
Enlarged supraclavicular lymph node and partially imaged massive tumour in the right breast.
The patient was non-compliant and attempted to abscond as soon as the infection improved with intravenous Flucloxacillin, despite explanation of its risks. In light of the patient’s non-compliant behaviour and risk of being lost to follow-up, preoperative biopsy of lymph nodes was thus abandoned, and the decision was made for a semi-urgent surgery. Informed consent was obtained, and the patient underwent a right mastectomy and axillary clearance. Elliptical incision was made while preserving surrounding healthy tissue. The excised mass was 310 × 200 × 240 mm in size (Fig. 3). Level I and II axillary clearance was performed. Due to laxity of the skin, primary closure was achieved.

Histology of the excised mass demonstrated mitotic count of 7 out of 10 high-power field (HPF) with stromal overgrowth confirming the diagnosis of borderline PT with negative margins. A total of 25 lymph nodes were harvested, and all demonstrated reactive follicular hyperplasia.
The patient had an uneventful post-operative recovery and was discharged home. Her case was discussed in our centre’s multidisciplinary meeting, and the consensus was for surveillance with annual mammography, and 6-monthly clinical follow-up for 3 years, then annually thereafter. Of note, she only attended a single post-operative appointment and there were no further follow-up appointments as she was not contactable.
DISCUSSIONS
Data are scarce on giant PT and most of the cases are from developing countries. The infrastructure and resources for routine screening mammography are often sparse in developing countries and thus leading to PT being diagnosed at a later stage and gigantic size. In contrary to developed countries, the population is well educated; therefore, cancers are commonly found at an early stage. Undoubtedly, it is rare to encounter such an extreme case.
Diagnosis of PT remains a work in progress. Core needle biopsies have been used extensively in the diagnostic workup of breast lesions [4]. However, the role of core needle biopsy in diagnosing PT and differentiating it from stromal tumours remains unclear, given the relatively high false negatives and false positive rates [5]. The main differential diagnosis for our case includes PT, metaplastic carcinoma and mesenchymal tumours such as atypical/malignant solitary fibrous tumour. Due to the overlapping histological features, the pathological diagnosis of PT in the present case was made on the examination of the surgical specimen.
The National Comprehensive Cancer Network guideline has recommended wide excision with margins ≥1 cm and axillary lymph node clearance is not required [6]. However, in our case, wide excision was not achievable due to the significant size of the tumour, with the entire breast parenchyma being replaced by the stromal tumour and negative resection margins was impossible to achieve without a mastectomy [7, 8]. Clinically, the lymph nodes were palpable and preoperative lymph nodes biopsy was not attainable due to patient factors and the dilemma of possible diagnosis of metaplastic carcinoma based on core biopsy. The decision to proceed for level 1 and 2 axillary clearance was made after discussion with the radiologist, given that the lymph nodes were highly suggestive of malignancy on imaging [9]. This again outlines the complexity of managing rare gigantic PT in a patient who is non-compliant and at high risk of absconding. Clinicians should cater management on a case-by-case basis taking patient factors into consideration.
Given the rarity of the disease, the validity of adjuvant radiotherapy and chemotherapy are often not evidence based. The role of chemotherapy is debatable based on a small observational study, whereas radiotherapy should be reserved for patients with malignant tumour and positive surgical margins [10].
In conclusion, there needs to be emphasis on continued efforts to narrow the educational gap in preoperative tissue diagnosis and post-operative care of patients in particular with rare conditions, which present atypically, such as PT.
AUTHORS’ CONTRIBUTION
Y.T.S. contributed in designing and writing of manuscript. B.K. reviewed and critically analysed the manuscript. Both the authors have approved the final version of this manuscript.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICAL APPROVAL
No ethical approval is required to publish this case report.
CONSENT
Patient consent was obtained.
GUARANTOR
The corresponding author will accept the full responsibility of the work.



