-
PDF
- Split View
-
Views
-
Cite
Cite
Murad Tarmohamed, Abednego Mashambo, Adnan Sadiq, Alex Mremi, Kondo Chilonga, Ectopic uterus? A rare presentation of a giant leiomyoma in the posterior mediastinum, Journal of Surgical Case Reports, Volume 2021, Issue 12, December 2021, rjab584, https://doi.org/10.1093/jscr/rjab584
Close - Share Icon Share
Abstract
Leiomyomas are benign mesenchymal tumors derived from smooth muscles. Uterus is the commonest site of origin for leiomyomas; however, unusual growth patterns and locations have been reported posing diagnostic challenges, clinically and radiologically. Histological diagnosis remains the gold standard of diagnosis. Here, we present a 17-year-old female with a 3-month history of chest pain, cough, difficulty in breathing and chest tightness. Chest CT scan showed a 12.3 cm × 14.4 cm × 22.8 cm mass occupying the entire left posterior hemithorax. The patient underwent thoracotomy and recovered well after surgery. Histopathology of the excised specimen confirmed it to be leiomyoma. Despite its rarity, primary mediastinal leiomyoma should be considered in the differential diagnosis of an unexplained mediastinal mass. Its accurate pre-operative diagnosis is difficult. Respiratory compromise and risk of transformation to sarcoma mandate complete surgical resection for a definitive diagnosis and good prognosis.
INTRODUCTION
Leiomyoma is a benign mesenchymal tumor derived from smooth muscles [1]. Leiomyoma commonly originates in the uterus, however, in rare occasions unusual growth patterns and anatomical locations can occur, challenging their identification clinically and radiologically [2]. Primary leiomyomas occurring in the mediastinum are extremely rare. They are usually slow-growing tumors and often detected incidentally on chest radiographs [3]. In this report, we present a 17-year-old girl with a giant leiomyoma in the posterior mediastinum, who underwent successful surgical resection.
CASE PRESENTATION
In March 2021, a 17-year-old female from Kilimanjaro region presented with a 3-month history of gradually progressive left-sided chest pain associated with cough, difficulty in breathing and chest tightness. The pain was worse on lying on the affected side. No history of hemoptysis, fever, night sweats or weight loss, neither exertional dyspnea nor orthopnea reported. No contact with tuberculosis reported. No significant past medical history. She does not use tobacco or alcohol. Upon examination, she was comfortable at rest and saturating at 99% in room air. Her axillary temperature, pulse rate and blood pressure were 36.4°C, 100 beats per minute and 116/79 mmHg, respectively. On chest examination, trachea was deviated to the right and there was reduced air entry on the left side. Apex beat was at fifth intercostal space mid-clavicular line and s1 and s2 sounds were heard with no added sounds. Other systems were unremarkable. Her hemoglobin level was 12.9 g/dl; serum creatinine of 72 μmol/l; prothrombin time and international normalization ratio were 11.3 and 0.89 seconds, respectively. Serum electrolytes were within normal range.
An initial chest radiograph of the patient confirmed tracheal deviation and revealed a mass in the left hemithorax. Chest CT scan (Fig. 1) showed a large mass occupying the entire left posterior hemithorax measuring 12.3 cm (AP) × 14.4 cm (T) × 22.8 cm (CC) with associated partial collapse of the left lung and mediastinal shift to the contralateral side suggestive of pleuropulmonary blastoma vs. neurogenic tumor (ganglioneuroma). This was followed by a CT-guided core needle biopsy which revealed benign spindle cells on a myxoid background. Abdominopelvic ultrasound was normal.
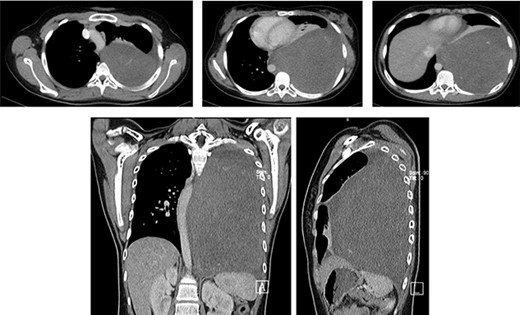
Axial, coronal and sagittal chest CT soft tissue window shows a large mass occupying the entire left posterior hemithorax measuring 12.3 cm (AP) × 14.4 cm (T) × 22.8 cm (CC) with associated partial collapse of the left lung and mediastinal shift to the contralateral side; the mass abuts to the descending aorta. No evidence of rib or thoracic spine destruction seen.
We performed a left-sided sixth-interspace thoracotomy. Intra-operatively, we found a huge, firm mass in the posterior mediastinum arising from the parietal pleura adjacent to thoracic vertebrae and fixed to the posterior ribs and intercostal muscles. The mass was in close proximity to the descending aorta from which it had one main feeder vessel. The left lung was collapsed yet normal. The tumor was excised and weighed 2.4 kg. The specimen (Fig. 2) was submitted for histopathology examination (Fig 3 and 4). The left lung was inflated and expanded normally.

A well circumscribed tumor which is non-capsulated with firm white cut surface; neither hemorrhage nor necrosis noted.
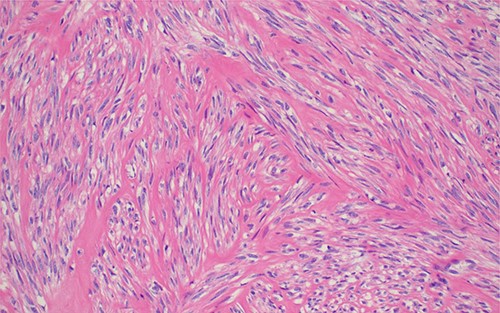
Histopathology of the lesion demonstrating monotonous population of spindle shaped cells in intersecting fascicles without cytological atypia; H&E stained sections 100× original magnification.
Post-operatively, the patient was monitored in ICU and kept on parenteral ceftriaxone 1 g and gentamicin 80 mg 12-hourly, paracetamol 1 g 8-hourly and pethidine 25 mg 6-hourly. She was extubated on post-operative Day 1 and transferred to general ward on the second day. The patient was discharged on 9th post-operative day. She was followed up at the surgical outpatient clinic at 2, 4 and 6 weeks post-operation where she reported full recovery and had normal findings on physical examination and chest X-ray (Fig. 5).
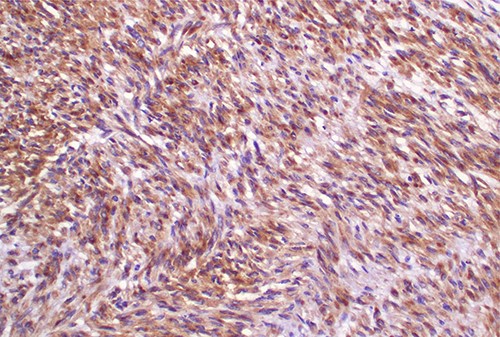
Photomicroscopy of the lesion highlighting positive immune-reactivity of the tumor cells with desmin immunostaining; IHC stained section 200× original magnification.

Chest X-ray (PA) shows no mass in the left hemithorax after thoracotomy and tumor resection; chest tube in situ; heart and lungs appear normal.
DISCUSSION
Primary Mediastinal Leiomyoma (PML) is rare, and only few cases have been reported in literature.
Its diagnosis can be incidental for non-symptomatic patients or intentional for symptomatic patients on a chest radiography. The manifestation of symptomatic mediastinal leiomyoma is attributed to the mass effect onto the adjacent mediastinal structures. Generally, the leiomyoma size is large at the time of diagnosis owing to its gradual growth without symptoms until pressure effect occurs. Symptoms commonly manifest as dyspnea, dysphagia or superior vena cava syndrome [3, 4].
Preliminary diagnosis is enhanced by a chest CT defining the mass (solitary, well-circumscribed tumor with heterogeneous density), size, location, blood supply and its relation to the adjacent vital mediastinal organs [3, 5]. Some tumors can develop degenerative changes such as hemorrhage, cystic changes and calcifications [6]. Based on the findings and age of the patient, pleuropulmonary blastoma and neurogenic tumor (ganglioneuroma) may be considered for differential diagnoses.
Complete resection is sufficient treatment of PML, regardless of its symptom status [4]. In this patient, the left posterior mediastinal leiomyoma was attached to the posterior thoracic wall (parietal pleura), with a pedicle of about 10 × 10 cm. While the mass encased part of the descending aorta, there was no local invasion of any mediastinal vital organs. Despite the pedicle’s small size relative to the large leiomyoma, it was firmly attached to the thoracic wall and hard; not easily dissectible. The lung was almost completely collapsed but regained near complete expansion and full function on spontaneous breathing within 24 hours.
The definitive diagnosis is achieved by histology. Microscopically, leiomyoma consists of monomorphic spindle cells with blunt-ended nuclei, arranged in interlacing fascicles, without atypia, mitosis or necrosis [4, 6, 7].
Due to rarity of this entity, two different high institute pathology laboratories were used to confirm the diagnosis.
After complete surgical resection of mediastinal leiomyoma, the prognosis is excellent and local recurrence is uncommon [5]. In case of recurrence, leiomyosarcoma should be considered [4]. Leiomyoma is often considered as benign tumor with a low malignant potential; however, there is need for strict follow-up because of reported metastasis [3, 6, 8].
CONCLUSION
Despite its rarity, PML should be considered in the differential diagnosis of an unexplained mediastinal mass. Its accurate preoperative diagnosis is challenging. Due to risk of continual growth and mass effect and risk of transformation to leiomyosarcoma, the recommended modality of treatment is complete surgical resection whether symptomatic or asymptomatic, for a definitive diagnosis and good prognosis.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the consent is available on record.
AUTHORS’ CONTRIBUTIONS
All authors contributed equally to this manuscript.
ACKNOWLEDGEMENT
The authors would like to thank the patient for giving their consent for their information to be shared for further learning purposes.
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interests to disclose.
References
- respiration
- chest pain
- smooth muscle
- inspiration
- cough
- differential diagnosis
- fibroid tumor
- respiratory insufficiency
- sarcoma
- surgical procedures, operative
- thoracotomy
- diagnosis
- mediastinum
- neoplasms
- uterus
- chest ct
- mediastinal mass
- excision
- gold standard
- chest tightness
- histopathology tests
- posterior mediastinum



