-
PDF
- Split View
-
Views
-
Cite
Cite
Ismail Mahmood, Mohammad Kasim, Ayman El-Menyar, Syed Nabir, Ibrahim Afifi, Husham Abdelrahman, Sandro Rizoli, Hassan Al-Thani, Late development of giant hepatic artery pseudoaneurysm following abdominal trauma due to tire blast: case report and literature review, Journal of Surgical Case Reports, Volume 2021, Issue 12, December 2021, rjab564, https://doi.org/10.1093/jscr/rjab564
Close - Share Icon Share
Abstract
Giant hepatic artery pseudoaneurysm is rare but could have a significant implication. A 35-year-old male was severely injured by a truck tire explosion and presented with hypotension and positive focused assessment with sonography in trauma scan. After resuscitation, abdomen computed tomography (CT) scan showed a Grade 4 liver injury. The patient was admitted to the intensive care unit, and the liver injury was treated conservatively. Seventeen days later, he developed abdominal pain with deep epigastric tenderness. Repeated abdomen CT scan detected a giant hepatic artery pseudoaneurysm. Embolization was achieved using gel foam with the placement of six microcoils. The patient had an uneventful recovery. Late development of giant hepatic artery pseudoaneurysm is a rare complication of hepatic trauma and could be life-threatening. Timely identification and treatment with endovascular intervention are crucial. We recommend, especially when dealing with trauma related to blast injury, follow-up images for patients who develop symptoms suggestive of hepatic injury.
INTRODUCTION
Giant hepatic artery pseudoaneurysm is rare and usually asymptomatic; however, it could have life-threatening complications, such as spontaneous rupture into peritoneal cavity or to the neighboring hollow organs [1]. The estimated incidence of hepatic artery aneurysms is 0.002%, and almost 50% of them are pseudoaneurysms [2]. Hepatic artery pseudoaneurysm has a risk of rupture, but its incidence is not yet well-reported. Moreover, blast trauma is not a common cause of such vascular lesion in the liver. We report a case of a young-old male who was severely injured by a truck tire explosion inside a garage. This case highlights the potential vascular hazards of unusual mechanism of liver injury and emphasizes the delayed presentation and management of hepatic pseudoaneurysm following blunt trauma.
CASE PRESENTATION
A 35-year-old male was severely injured by a truck tire explosion inside a mechanic garage. The EMS crew reported to the trauma team that the patient was found anxious, diaphoretic and hypotensive. Following fluid resuscitation, the patient was brought to the Level 1 trauma center. Upon admission, the patient’s initial vital signs were as follows: Glasgow coma scale: 15, blood pressure of 84/50 mmHg, heart rate of 117 beats/min; respiratory rate of 23 breaths/min and pulse oximetry of 99% under a reservoir mask oxygen flow of 10 l/min. There was tenderness and mild guarding in the right hypochondrium. Hemoperitoneum was identified on the focused assessment with sonography in trauma. Extremities examination revealed bilateral femur and right radius fracture (Fig. 1).

Radiographs show bilateral femoral and right radius fractures. R: right, L: left.

Repeated CT scan on Day 5 showing liver laceration with no evidence of hepatic pseudoaneurysm.
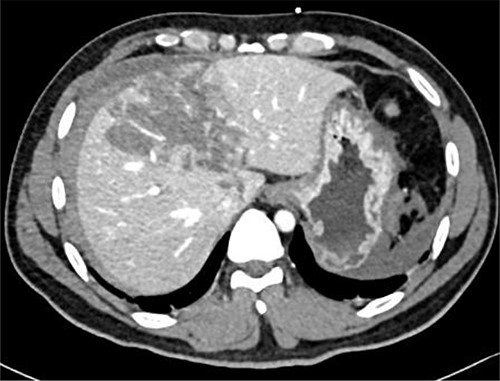
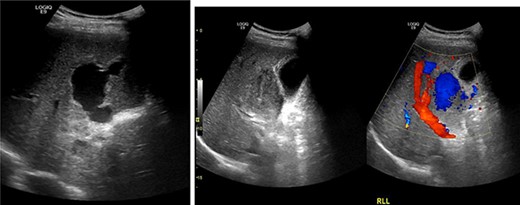
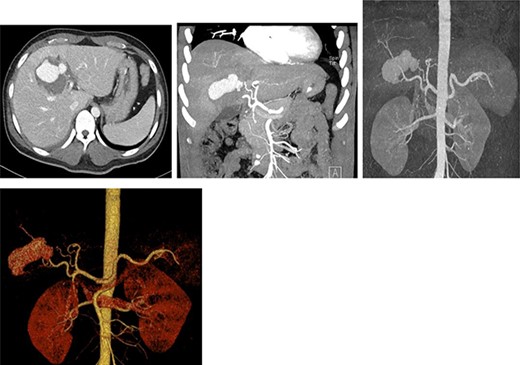
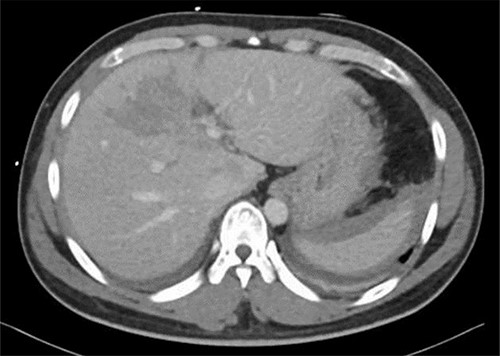
Resuscitation was carried on with 2 l of normal saline and two PRBC units to stabilize the patient. The computed tomography (CT) scan identified Grade 4 liver injury with hemoperitoneum (Fig. 2). Subsequently, the multiple bone fractures underwent surgical fixation, and post-operatively, he was hemodynamically stable. On the fifth day after admission, repeated CT scan demonstrated the liver injury with no evidence of hepatic pseudoaneurysm (Fig. 3). The patient remained stable with tolerated feeding with no abdominal pain or distension. On the Day 17, he developed abdominal pain mainly in the epigastrium, which was associated with nausea and deep epigastric tenderness. Abdominal ultrasound (US) (Fig. 4) and CT scan (Fig. 5) revealed complex, large intraparenchymal hepatic pseudoaneurysm (measuring about 58 × 41 × 30 mm) related to the left hepatic artery Segment 4 branch with surrounding hematoma located mainly at segment 4B/A ,and there was another tiny pseudoaneurysm seen at Segment 4A. Selective angiography confirmed the diagnosis of pseudoaneurysm with multiple blood supplies from Segment IV and Segment II.
Contrast-enhanced CT scan revealing a right hepatic artery pseudoaneurysm in the right lobe of the liver.
Embolization was achieved using gel foam and particle (embosphere: 100–300 mic) through microcatheter until satisfactory stagnation of forward flow was reached and back flow was seen. Then, the aneurysm was occluded with placement of six microcoils (3 and 5 mm) (Fig. 6).
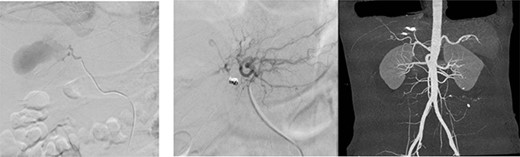
(a) Arteriogram showing a hepatic artery pseudoaneurysm in the right hepatic artery; (b) shows post-embolization selective arteriogram showing disappearance of the pseudoaneurysm in the right lobe of the liver; CT angiogram shows successful embolization (c).
After 1 week of embolization, a follow-up CT scan detected thrombosis of the lateral segmental branch of the left portal vein. Prophylaxis dose of heparin was increased to the therapeutic range and, a week later, duplex US examination was performed, which documented the resolution of this thrombosis. The patient was transferred to the rehabilitation care on daily oral aspirin. A repeat CT scan was done after 1 month in which no pseudoaneurysm was seen, with normal flow in the hepatic arteries and portal vein (Fig. 7). During the following 2 months, the patient remained asymptomatic and was discharged home without complications.
Repeated CT scan of the abdomen after 4 weeks revealed partial healing of the liver injury with disappearance of the pseudoaneurysm.
DISCUSSION
The high-level energy generated by exploding tires (which classified as a barotrauma) could produce high pressure, causing damage to body tissues or internal organs. In addition, it may lead to direct injuries as a result from the body being thrown against the floor, wall or other hard objects [3]. Hepatic injury in a primary blast wave can be subcapsular hematoma, contusion or laceration, which can be isolated or associated with other body organ injuries. Damage can be present on any surface of the liver, depending primarily on the area hit by the blast wave [4].
A hepatic pseudoaneurysm is a false aneurysm that develops from a leak of a damaged artery into the adjacent tissues, forming a cavity beside the artery. It can be recognized from intrahepatic hematoma as it continues to communicate with the artery, causing a high-pressure cavity with the risk of rupture [5]. Giant visceral pseudoaneurysms are aneurysmal lesions of the splanchnic vessels that are >5 cm in diameter [6]. Post-traumatic hepatic artery pseudoaneurysm is uncommon, appearing in ~1–4% of hepatic trauma cases; 80% of the cases are extrahepatic [7]. It may occur because of blunt or penetrating abdominal trauma [8].
The diagnosis of hepatic artery aneurysm is made with either conventional angiography, CT-angiography or Doppler US [5]. On CT imaging, hepatic artery pseudoaneurysm is identified as a well-defined focal lesion of high attenuation with the same contrast enhancement as arterial structures [5]. In our case, hepatic artery pseudoaneurysm diagnosis was established with abdominal CT scan and was confirmed with hepatic angiography. Like the management of blunt splenic trauma in adults, the treatment of post-traumatic liver injury remains controversial. Some physicians believe that routine follow-up imaging is necessary in all cases of post-traumatic liver pseudoaneurysm because of the risk of disastrous hemorrhage, while others believe that they can simply be observed as spontaneous resolution is known to occur.
Prior study of 530 hepatic trauma patients by Cox JC et al. [9] documented that only 3 patients with hepatic injury required an intervention because of a repeated CT scan; therefore, they concluded that routine follow-up imaging was not required because it did not change patient management. However, follow-up images are suggested for patients who develop signs or symptoms suggestive of active hepatic abnormality.
Similarly, Pachter et al. and Bertens et al. [10, 11] reported that no clear advantage was obtained from repeated follow-up CT scans. Conversely, a recent large study by Wagner et al. [12] documented that 18 patients out of 600 trauma patients had hepatic pseudoaneurysm. Seven pseudoaneurysms were found on asymptomatic surveillance CT angiography, and 11 patients were symptomatic at the time of scan surveillance. Of the 11 symptomatic patients, 4 were in hemorrhagic shock, and 2 died from hepatic-related complications. The author concluded that aggressive surveillance for hepatic pseudoaneurysm with interval CT angiography may be reasonable, especially for Grades IV and V injuries.
Comparably to the last study, Østerballe et al. [13] reported 4% incidence of hepatic pseudoaneurysm, which was not correlated with the grade of liver injury. They concluded that a routine follow-up imaging was reasonable to prevent life-threatening hemorrhage.
The optimal time frame for follow-up CT in patients with liver injuries was unknown. Some authors suggested 24–48 h after abdominal blunt injury [11]. However, others recommended 5 and 7 days from the original trauma [12]. In the current case, initial follow-up CT scan angiography on the fifth day after the injury did not identify pseudoaneurysm. A repeated CT scan after 17 days discovered late development of giant hepatic pseudoaneurysm. This late formation of pseudoaneurysm could be related to the combination of blunt trauma and high energy generated by the blast overpressure of tire explosion.
CONCLUSION
Late development of giant hepatic artery pseudoaneurysm is a rare complication of hepatic trauma and could be life-threatening. Timely identification and treatment with endovascular intervention is crucial. We suggest, especially when dealing with trauma related to blast injury, follow-up images for patients who develop symptoms suggestive of ongoing hepatic injury.
Funding
None.
CONFLICT OF INTEREST STATEMENT
All authors declared no conflict of interest.
ETHICS APPROVAL
Data were collected retrospectively and anonymously. Ethical approval to report this case was obtained from the Medical Research Center at Hamad Medical Corporation, Doha, Qatar, provided that no patient-identifiable data are included (MRC-04-21-571).
References
Tipaldi MA, Krokidis M, Orgera G, Pignatelli M, Ronconi E, Laurino F, et al.
Francisco LE, Asunción LC, Antonio CA, Ricardo RC, Manuel RP, Caridad MH.



