-
PDF
- Split View
-
Views
-
Cite
Cite
Niloofar Sherazi Dreyer, Lina Pankratjevaite, Dainius Janciauskas, Zilvinas Saladzinskas, Rare case of visceral myopathy, Journal of Surgical Case Reports, Volume 2021, Issue 12, December 2021, rjab554, https://doi.org/10.1093/jscr/rjab554
Close - Share Icon Share
Abstract
Visceral myopathy is a rare bowel disease affecting peristalsis and causing pseudo-obstruction. There is no specific treatment for chronic intestinal pseudo-obstruction caused by visceral myopathy. We report a case of a 30-year-old woman with visceral myopathy who, due to unsuccessful conservative treatment, underwent surgery. However, few surgeries did not give the desired result and the patient still suffers from chronic constipation, abdominal distension and pain. The diagnosis of visceral myopathy is complicated. Neither conservative nor surgical treatment of visceral myopathy is associated with good results.
INTRODUCTION
Visceral myopathy is a rare and often misdiagnosed disease [1]. It affects peristalsis of the bowels and causes pseudo-obstruction [1]. There is no specific treatment for chronic intestinal pseudo-obstruction caused by visceral myopathy [2]. Surgical treatment is an option in patients who do not respond to conservative treatment [3]. In such cases, decompressive surgery might be used to relieve the symptoms [3]. Surgical resection in non-localized disease has disappointing results since the bowel affection is progressive and extends proximal to the resected line [3]. In line with the Consensus-based Surgical Case Report Guideline criteria, we report a case of a 30-year-old woman with visceral myopathy [4].
CASE REPORT
A 30-year-old woman presented to our hospital with a 10-year history of abdominal distension, constipation and intermittent abdominal pain. She used laxatives and enemas. Her past medical history was significant for pancreatic surgery. Five years earlier, she underwent segmental pancreatic resection because of solid pseudopapillary neoplasm. Her family history was negative for gastrointestinal, neurologic or other familial diseases.
The patient was hospitalized several times due to partial bowel obstruction, which was managed conservatively. Abdominal radiographs and computed tomography (CT) scans revealed diffused dilated loops of small and large bowels (Fig. 1). Colon transit time was measured using radiopaque marker test. All markers remained in the bowels 5 days after the ingestion of them. Colonic hypomotility was diagnosed. As the patient was incapacitated by symptoms and did not respond to conservative treatment, subtotal colectomy was performed. Histopathological examination revealed abnormal layering of colonic muscularis propria. Both inner and outer muscular layers were very thin and inadequate (Fig. 2). Nevertheless, the symptoms of pseudo-obstruction persisted and the patient underwent another surgery. Sigmoid resection with preventive ileostomy was done. Histopathological examination showed the same abnormal changes of the colonic muscular layer. Few months later, preventive ileostomy was closed and ileorectostomy was performed. However, adhesive post-operative small bowel obstruction complicated patient’s recovery. Relaparotomy and adhesiolysis were done. After the last surgery, the patient still complained of abdominal distension and constipation. Colonoscopy disclosed anastomotic stricture, ~5 mm in diameter (Fig. 3). Endoscopic dilation was done, but the patient complained of the same symptoms few weeks after the procedure. Endoscopy was performed again and it showed an anastomotic stricture. Endoscopic dilation was done. This procedure was repeated with stent placement for a few more times due to recurrence of anastomotic stricture. Moreover, the patient still complains of constipation. Constipations are associated with abdominal distension and pain and just laxatives and enemas bring some relief for the patient. The patient continues follow-up and endoscopic treatment (repetitive dilatations) at a medical centre in the USA.
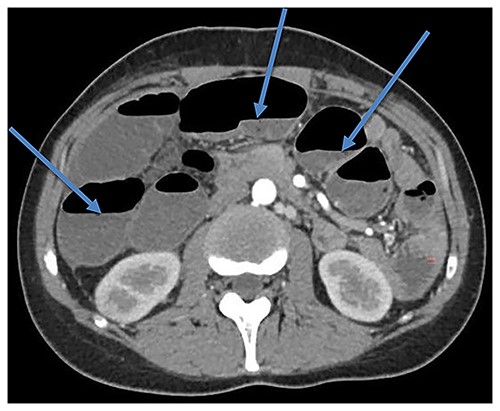
CT scan showing bowel dilatation (air-fluid levels are marked with arrows).
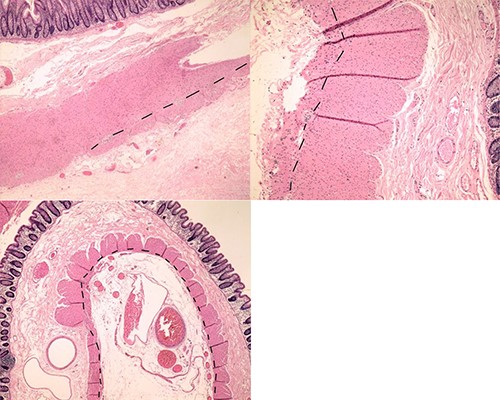
Histopathological examination showing abnormal changes of colonic muscular layer; particularly, abundant areas with minimal development of the outer muscular layer (dashed line shows the boundary between the muscular layers).
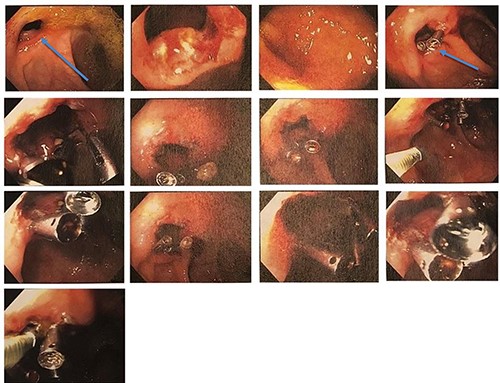
Colonoscopy disclosed anastomotic stricture, ~5 mm in diameter (labelled with an arrow); endoscopic dilation was done.
DISCUSSION
Visceral myopathy is a rare pathological condition of unknown aetiology. It is characterized by impaired intestinal function and motility in the absence of mechanical obstruction due to abnormal smooth muscles in the bowel. The disease is part of a group of pathological abnormalities called chronic idiopathic intestinal pseudo obstruction [5]. The condition can be inherited, idiopathic or secondary to other diseases, such as endocrine disorders, scleroderma, systemic lupus, amyloidosis, Ehlers- Danlos syndrome, stroke or encephalitis, drugs and toxins [5, 6].
Symptoms can present in paediatric as well as in adult populations, however, 80% of the patients present symptoms from the first month to the first year of life [7]. Clinical manifestations are nonspecific and may vary widely. Diagnosis is usually delayed and complicated. Some patients may be asymptomatic, and others may have a long history of gastrointestinal symptoms, such as abdominal pain, distension, nausea, constipation, vomiting or loose stools [6]. Multiple causes can trigger exacerbation of visceral myopathy disease [6].
Diagnostic criteria include absence of mechanical obstruction and histological examination of all intestinal layers [8]. To exclude mechanical bowel obstruction plain abdominal radiography, CT, magnetic resonance imaging or, in some cases, endoscopic examination might be used [7, 9]. Histopathological examination reveals degenerative changes of myocytes, fibrosis and partial or complete defects in the intestinal lamina muscularis propia [6, 8].
Manometry evaluation is more sensitive than imaging; it helps to evaluate the intensity and coordination of digestive tract and differentiate whether the intestinal dysmotility is due to neuropathic or myopathic pathophysiology [6].
Other gastrointestinal diseases such as Hirschsprung’s disease, pseudo-Hirschsprung’s disease, progressive systemic sclerosis involving gut, leiomyomatosis/angio-lymphangioleiomyomatosis, age-related neuropathies/musculopathies and segmental absence of intestinal musculature should be considered as differential diagnosis of visceral myopathy [5].
The management of visceral myopathy is challenging due to its rarity. No evidence-based guidelines for the treatment of visceral myopathy exist.
In idiopathic or primary visceral myopathy, treatment should involve fluid and electrolytes by intravenous infusions and both gastric and intestinal decompression by nasogastric/rectal tubes or tube replacement in a stoma [7]. In some cases, medicines such as erythromycin, octreotide or cisapride may be used to stimulate intestinal contractions [7, 9]. Surgical resections may be chosen when conservative treatment fails or when visceral myopathy is localized (affects a segment of the gastrointestinal tract) [1]. Nutritional support (orally, enterally or parenterally) is recommended. Approximately, two-thirds of the patients with CIPO have insufficient nutritional intake and may experience significant weight loss [7].
In our case, neither conservative treatment nor surgery has given satisfactory results.
CONCLUSION
The diagnosis of visceral myopathy is complicated. Visceral myopathy may mimic other GI disorders.
It is important to consider visceral myopathy diagnosis in patients with long-lasting or recurrent episodes of abdominal distension without evidence of mechanical obstruction, constipation and intermittent abdominal pain. Moreover, aggressive surgical treatment of patients with visceral myopathy-caused chronic intestinal pseudo-obstruction might be associated with poor results.
The condition affects the quality of life negatively and the prediction of prognosis is rather difficult. The treatment of visceral myopathy should be individualized, though no evidence-based standard treatment exists due to its rarity.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



