-
PDF
- Split View
-
Views
-
Cite
Cite
Nawaporn Kittaweerat, Worapat Attawettayanon, Teeranop Choorit, Virote Chalieopanyarwong, Choosak Pripatnanont, Pattama Tana-anantarak, Pornsak Dissaneewete, Bilateral renal fungal bezoars in a preterm infant: case report and literature review, Journal of Surgical Case Reports, Volume 2021, Issue 10, October 2021, rjab436, https://doi.org/10.1093/jscr/rjab436
Close - Share Icon Share
Abstract
Renal fungal bezoars or fungal balls is a rare condition in neonates and infants, usually occurring in immunocompromised patients. Renal bezoars result from accumulations of fungal cells and renal epithelial cells. The most common manifestation is candiduria, which can cause urinary tract obstruction. The treatment of choice is prompt medical or surgical intervention, as indicated to eliminate the infection and preserve renal function. Herein we report the case of a 34-week preterm male infant who presented with feeding intolerance, fever, acute kidney injury and alteration of consciousness. His initial creatinine was 3.4 mg/dL and urine analysis showed pyuria and yeast cells. A renal ultrasound demonstrated a dilated bilateral renal pelvis and calyx with bilateral fungal bezoars. The management was intravenous fluconazole with bilateral nephrostomy tubes and later surgical removal of bilateral fungal balls.
INTRODUCTION
Candidiasis causes urinary tract infection by hematogenous spread or ascending process. Most kidney infections or renal involvement occur from hematogenous spreading [1]. This is a relatively rare condition in infants [2] with predisposing factors of prolonged antibiotic use, prematurity, umbilical artery catheterization, parenteral nutrition and/or immunocompromised state [3]. Candida species occupy the gastrointestinal tract, genital tract and/or skin. Most Candida species cannot grow in urine except in patients with predisposing factors. Candida albicans is the most common species and accounts for 50–70% of all Candida-related urinary tract infections, followed by Candida glabrata and Candida tropicalis [4]. Many other fungal isolates have been described in the literature including Aspergillus spp., Mucormycetes spp., Cryptococcus spp., Histoplasma spp., Rhizopus oryzae and Geotrichum candidum [5, 6].
In children with disseminated candidiasis, the kidney is the most commonly involved organ. Fungal bezoars may also form in the renal pelvis and create a urinary obstruction in some children [7]. Renal ultrasonography is an essential tool for evaluating this condition [8]. Urinary alkalization and systemic antifungal therapy may successfully dissolve some fungal balls but percutaneous or surgical removal maybe necessary for cases suffering from renal obstruction or failure of systemic antifungal therapy [9].
CASE REPORT
A 34-week preterm male infant was delivered by cesarean section due to fetal distress. He was admitted to the neonatal intensive care unit (NICU) due to neonatal sepsis and mild acute respiratory distress syndrome. He received gentamicin and amikacin for a week despite his hemoculture, sputum culture and urine culture revealing no growth. His clinical condition improved following treatment. Twenty-one days later he developed feeding intolerance, oliguria, a history of non-foul-smelling diarrhea, fever and alteration of consciousness. A physical examination found a body temperature 39.3°C, tachycardia and tachypnea. Laboratory examinations showed hyponatremia (Na 119 mEq/L), hyperkalemia (K 10.5 mEq/L), metabolic acidosis (HCO3 11 mEq/L) and azotemia (BUN 31.6 mg/dL) with acute kidney injury (Cr 5.1 mg/dL). The urinalysis revealed pyuria and yeast cells. Urine and hemoculture demonstrated C. albicans. The patient was transferred to the Pediatric Intensive Care Unit, where ultrasonography demonstrated a dilated renal pelvis and calyx in both kidneys and bilateral echoic lesions with central hyperechoicity, suggestive of fungal bezoars (Fig. 1) and a large amount of ascites. He was given intravenous fluconazole, normal saline boluses, potassium correction, sodium bicarbonate boluses and ultrasound-guided ascites aspiration was performed. After resuscitation and initial treatment, his serum creatinine decreased to 1.22 mg/dL and his blood culture was negative, however, urine culture continued to show the presence of C. albicans. Re-imaging showed bilateral complicated perinephric fluid collections and a large number of intra-abdominal fluid collections. The patient underwent a bilateral percutaneous nephrostomy. An antegrade pyelography found a filling defect in the bilateral pelvocalyceal system with contrast extravasation at the upper and lower poles of the left kidney (Figs 2 and 3), following which his creatine improved to 0.37 g/dL. After that, the patient underwent a left pyelotomy (flank incision) with bezoar removal and PCN replacement with a left double J stent. Two weeks later, we performed an open right pyelotomy and double J stent insertion via a flank incision. After the operation, his symptoms improved and his creatinine decreased to 0.27 mg/dL. Tissue pathology from the renal pelvis revealed fungal balls consisting of Candida spp. (Fig. 4). After 167 days of admission, he was discharged from the hospital with serum creatinine of 0.30 mg/dL.
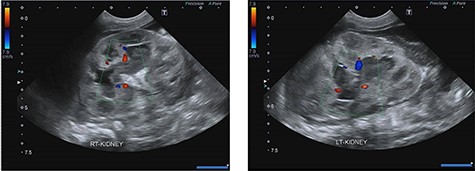
Ultrasonography shows echogenic lesions in dilated renal pelvis and calyces, bilaterally.

Antegrade pyelography; filling defect in the left kidney and contrast extravasation at the upper and lower pole.
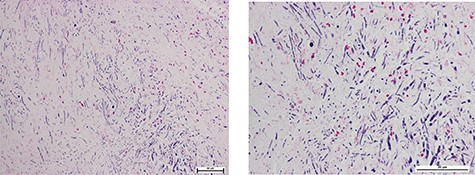
Pathological diagnosis report of fungal balls, consisting of Candida spp.

DISCUSSION
Upper urinary tract fungal infection and fungal bezoars are relatively uncommon. Fungal bezoars are formed by localized clusters of pseudomycelia. It should be considered in patients who are diagnosed with funguria or candidemia concomitant with renal insufficiency, oliguria or anuria [9].
In suspected patients, prompt ultrasonography of the urinary tract should be performed. The mainstay treatment of renal fungal bezoars is systemic antifungal therapy with fluconazole, which is effective in most cases because of good tissue penetration and high urine concentrations [10]. Invasive interventions such as nephrostomy tube insertion or surgical interventions to drain the kidneys are sometimes considered in patients with complete urinary obstruction. However, nephrostomy tube placement can be a technical challenge, especially in pre- and dysmature neonates, and nephrostomy tube displacement or obstruction by the fungal bezoars may lead to suboptimal treatment [11]. Antegrade amphotericin B or fluconazole via a nephrostomy tube has been reported to have good results in previous studies [7, 12]. This patient presented with bilateral fungal bezoars with urinary obstruction. The patient received systemic treatment with antifungal medication. After systemic treatment, imaging found perinephric fluid and large amount of ascites. Urinary drainage is required to relief obstruction and bilateral percutaneous nephrostomy is the procedure of choice. Local irrigation via nephrostomy with antifungal therapy showed evidence of improvement in the appearance of renal bezoars. Unfortunately, these were not tried in our patient due to a preliminary antegrade pyelogram finding of contrast media extravasation. This patient has poor clinical response to conservative treatments and failure of regression of fungal ball. Open pyelotomy with fungal ball removal was the next choice of treatment. Concerning about contamination and spread of infection, we decided to perform retroperitoneal approach. Patient underwent the first operation on the left side as the imaging study showed more severe obstruction and staged operation on the contralateral kidney was performed 2 weeks later.
Our report suggests that surgical removal might be effective and safe in patients with failed conservative treatment. The mainstay treatment of renal fungal bezoars is systemic antifungal therapy. However, the urinary obstruction prevented us from trying medical treatment and a decision was made to perform open surgery. Successful urinary drainage in this case was a time-buying strategy to give a long course of antifungal agents.
In conclusion, we demonstrated a case of bilateral fungal balls in a case of systemic candidiasis which caused obstructive uropathy. Sequential removal of the bezoars successfully relieved the obstruction.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
Abdeljaleel OA, Alnadhari I, Mahmoud S, Khachatryan G, Salah M, Ali O, et al.
- renal function
- consciousness disturbance
- candiduria
- creatinine
- renal failure, acute
- fever
- bezoars
- fluconazole
- immunocompromised host
- infant
- newborn
- infant, premature
- calyx
- renal pelvis
- pyuria
- surgical procedures, operative
- urinalysis
- yeasts
- infections
- kidney
- urinary tract obstruction
- epithelial cells
- renal ultrasonography
- nephrostomy
- excision
- feeding intolerance



