-
PDF
- Split View
-
Views
-
Cite
Cite
Benjamin Maurice Jones, Luke Nugent, Stuart James Griffin, Femoral condylar locking compression plates: a case series. The Rural District General Hospital Experience, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa380, https://doi.org/10.1093/jscr/rjaa380
Close - Share Icon Share
Abstract
Most studies regarding the use of locking condylar plates in distal femoral fractures have been carried out in tertiary centres. The aim of this case series was to examine outcomes for patients managed in a rural setting and to answer the question: ‘should we be shipping these patients out to a regional trauma centre?’ Recent insertions of condylar locking compression plates (LCPs) at a rural district general hospital were examined. (All used the Synthes LCP Condylar Plate 4.5/5.0 periarticular plating system). Their clinical records and radiology were reviewed to identify failure rates and facilitate discussion of such cases. Of 36 reviewed cases, 4 instances of failure were identified (11%), and their cases are discussed individually herein. This review not only affords the opportunity to discuss cases of failure and to speculate upon their potential causes, but also highlights reassuringly high quality of outcomes for these patients outside of larger teaching hospitals.
INTRODUCTION
Distal femoral fractures present surgeons with multiple challenges. Their incidence with age demonstrates bimodal distribution—young patients involved in high-energy trauma such as road traffic accidents and the elderly suffering low-energy falls. These older patients are often osteoporotic and co-morbid [1], and this injury traditionally conferred high morbidity and mortality. This is reflected in the fact that some units are now applying their well-developed femoral neck fracture management pathways and proformas to patients with fractures at the other end of the femur [2]. Intra-articular injuries require careful anatomical reduction to facilitate acceptable long-term outcomes, and all of these fractures must be managed in a way that restores the mechanical axis of the knee. In order to achieve this, with the exception of patients with minimally displaced fractures and those who are not fit surgical candidates, operative intervention is almost always called for. Historically, simple management techniques (traction, plaster immobilization, cast bracing, etc.) resulted in good union rates (in closed injuries), but these patients suffered from long-term knee stiffness, contractures and post-traumatic arthritides [3]. Early operative interventions took the form of either dynamic compression plate (DCP)-style plating techniques or intra-medullary nailing. Nails had achieved good results in diaphyseal fractures but were not compatible with more distal or comminuted fractures. Conventional plating techniques rely on the screws’ ‘purchase’ on the cortex to generate stability, in that the construct’s ability to resist axial deforming forces is dependent on screw torque (as well as mechanical friction between the plate and the bone) [4]. Such mechanical purchase is naturally limited in the osteoporotic subject, and the periosteal compression necessary in order to achieve this bone–plate friction coefficient has self-evident consequences for the fracture’s vascular supply. Modern distal femoral condylar locking plates have largely developed from Synthes’ Less Invasive Stabilization System (LISS), patented in Davos in 1990. These combined the fixed-angle rigidity of an intra-medullary nail locked above and below the fracture with the plate’s ability to hold anatomical reduction even in very distal injuries [5]. The result was an internal ‘external fixator’. Because the LISS plate was designed with a minimally invasive percutaneous osteosynthesis (MIPO) technique in mind, and also as the screws are locked in a fixed position, the diaphyseal segments had to match a generic femoral curvature (as the surgeon would not be able to angle the screws towards the central point of the femoral shaft wherever the fixator did not cover bone). However, the precise anatomical contouring needed in traditional plating was no longer required as these plates need not be compressed onto bone in order to achieve stability [6]. LISS plates were first used clinically in 1995 and preliminary results showed good outcomes [7]; however, certain fracture configurations still demanded the absolute stability generated by a DCP. As such, the Arbeitsgemeinschaft für Osteosynthesefragen (AO) locking compression plate (LCP) was developed with combination holes, permitting either modality to be used with a single system as the situation required or as an internal fixation system combining both techniques [8] (e.g. in a transverse mid-shaft femoral fracture where hip and knee arthroplasties exclude nailing). Their adaptability and multipurpose functionality have made them a popular and widely available implant choice. The potential for an overly rigid construct to become a ‘non-union generator’ was recognized at an early stage [9], and so surgeons were advised to pre-dynamize when using LCPs in a bridging mode by allowing at least two empty screw holes over the fracture gap. This decreases the internal stresses on the plate and effectively increases its working length [10]. The optimum screw ratio (number of screws inserted over available holes) for LCP in bridging mode (regardless of whether bicortical or unicortical screws are utilized) has been determined by biomechanical models to be 0.4–0.5 with three or four screws on either side of the fracture gap [11]. Taking the above into account reduces the risk of fatigue fracture of the plate.
A significant body of evidence has since been gathered to determine the efficacy of the LCP. In 2013 Ehlinger et al. [12] reviewed the available literature with regards to the various surgical techniques used to treat distal femoral fractures and concluded that while it was not without fault, the LCP was in principle the only option appropriate for the management of any distal femoral fracture.
METHODS
For this case series the 50 most recent distal femoral fractures treated with the Synthes 4.5/5.0 LCP condylar plate operated at Ysbyty Gwynedd District General Hospital (DGH) (North Wales) between 2014 and 2019 were assessed, prior to 6 months from commencing the study to allow for adequate follow-up. This rural DGH is a medium-sized 500 bed site serving a predominantly elderly population of roughly 100 000 people.
Fractures were categorized according to the AO classification based on retrospective review of presenting radiographs supplemented by computed tomography imaging when this was available. Medical records were then reviewed to facilitate the rest of the data collection.
Patient-specific data points were collected including patient age at procedure, the recorded American Society of Anesthesiologists (ASA) grade, presence of diabetes mellitus, smoking status, presence of pre-existing vascular disease and sex. Details regarding the surgical team were also recorded including the seniority of the named lead surgeon. Approach choice (direct lateral versus MIPO) was recorded, as well as the use of any supplementary metalwork (such as concomitant anterior plating or the use of cerclage wiring). Post-operative data points recorded were the length of follow-up (weeks), whether the patient was pain free at final follow-up and time to radiographic union (weeks) or failure/non-union were also recorded (weeks). In cases of failure details relating to further procedures were also recorded.
To facilitate meaningful comparison with recent similar studies, radiological union was defined as cross-trabeculation seen on both anteroposterior and lateral radiographs [13]. Non-union was defined as failure of fracture union at 9-month follow-up.
Clinic letters were reviewed, taking account of functional outcomes when available.
RESULTS
Mean age at presentation was 77.38 years, comprising of 40 women and only 10 men. Eight patients were diabetic, 20 were smokers and 10 had some form of pre-existing arterial vascular disease.
The assigned ASA scores were as follows: ASA I = 3 patients, ASA II = 9 patients, ASA III = 20 patients, ASA IV = 13 patients, not recorded = 5 patients.
A consultant was the lead surgeon in 28 cases (22 carried out by middle grades). Only one of the four cases of failure had a consultant as the named lead surgeon.
In total, 25 patients did not have a peri-prosthetic fracture at presentation, 10 patients had a hip prosthesis, 1 had a fracture at the distal pole of her femoral intra-medullary nail, 9 patients had a fracture about a knee prosthesis and 5 had a fracture lying between both hip and knee prostheses.
Presenting fracture types according to the AO classification (for patients without peri-prosthetic injuries) were recorded, the most common fracture patterns being AO 33A2.1 and 33A2.2.
Suction drains were not employed in any of the cases. Skin staples were used for closure in all but one case (where an absorbable monofilament suture was used). No bone grafting was performed. In-patient mobilization under supervision from a physiotherapist was employed from Day 2 in all cases (a physiotherapy-led recovery pathway being followed across the trust) with ‘partial weight bearing’ being advised throughout the cohort for 6 weeks, with patients being advised to wean themselves from the use of mobility aids thereafter. In total, 14 patients were lost to follow-up (7 patients were from out of area, 5 patients had died and 2 did not attend follow-up appointments).
Of the remaining 36 patients, 4 instances of failure were identified and their cases are discussed individually (below). No clear cases of non-union were noted; however, some of the failures could be attributed to an underlying non-union (see below), and one patient was discharged from follow-up before radiographic union had been appreciated due to good clinical outcomes and logistical difficulties in attending clinic follow-up. No cases of significant infections were identified; however, one patient did report some wound redness that settled with oral flucloxacillin provided by his general practitioner.
The mean time to radiographic union (for the 32 patients in which it was seen) was 31.5 weeks. Average length of follow-up was 43 weeks.
Two patients had elective removal of the plate due to ongoing pain following successful union (both roughly at the 2-year mark).
In total, 18 cases were carried out by MIPO technique (2 of the failures included in this group), the other 32 were carried out via direct lateral incisions.
In total, 30 of the followed-up patients (83%) reported that they were pain free prior to discharge from clinic.
DISCUSSION
High rates of loss to follow-up can largely be accounted for by a significant number of ‘out-of-area’ patients included in this cohort, the hospital in question serving the Snowdonia National Park. The mean age at presentation of 77.38 years may also be explained by the regions demographics and in itself may go some way to explaining the increased time taken for radiographic union to be demonstrated at follow-up.
A failure rate of 11% again is somewhat higher than has been reported in previous reviews [13–18] but may be explained by the aging population studied here.
The cases of failure are here examined in more detail. Case 1 (Figs 1 and 2): this active gentleman was paddleboarding off the Llŷn peninsula when he was knocked onto his side by a wave.
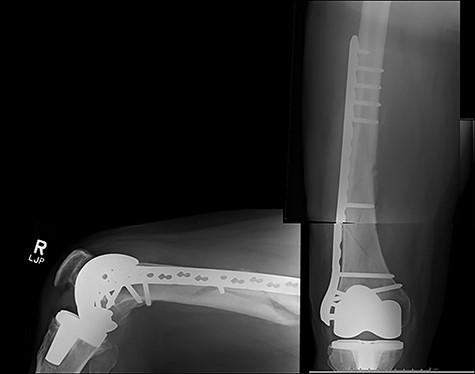
Fracture above plate tip following successful union for Case 1.
Clearly, this has occurred following on from successful union. Despite a sound original fixation, the rigid construct has acted as a lever-arm to produce a fracture above the plate tip. In long spiral fracture configurations such as this, antegrade intra-medullary nailing could be considered as the primary treatment modality.
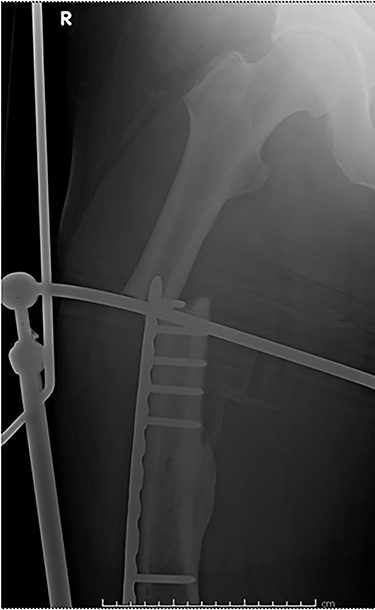
Case 2 (Figs 3–5): here difficulties were clearly encountered in achieving satisfactory reduction in the coronal plane. The screw immediately proximal to the fracture line is too close to the fracture.



Selecting a longer plate would have allowed proximal screws to sit more appropriately in order to reduce the risk of plate fatigue.
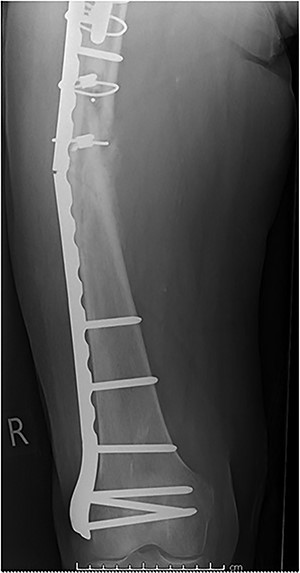
Case 3 (Figs 6 and 7): another case of fatigue fracture of the plate prior to bony union. Here cerclage wires close to the fracture site may have had the same effect as placing screws immediately adjacent to the fracture. It would seem reasonable to speculate that their exclusion may have led to a more satisfactory outcome.

Case 4 (Figs 8–10): once again, screw placement too close to the fracture site has resulted in internal plate stresses exceeding its load-bearing capacity.
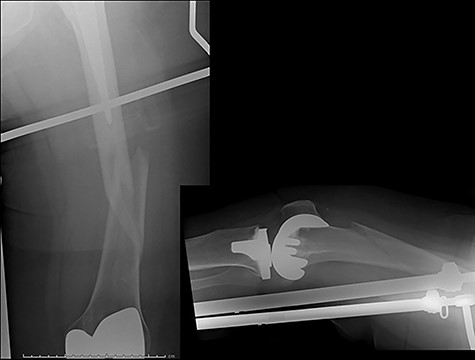


Inter-fragmentary screws have been utilized here. This lady may have benefited from placing an anterior bridging plate at the time of her original procedure if it was not possible to avoid this screw configuration.
This case series was not powered to detect statistically significant correlations between its recorded co-morbidities and failure rates, but no apparent trends seem to emerge from the available data.
This review has not only afforded the opportunity to discuss the above cases of failure and to speculate upon their potential causes, but also highlights the perhaps surprising frequency with which such procedures are carried out even in rural DGHs (one to two cases per month) and a reassuringly high quality of real-world outcomes for these patients outside of larger teaching hospitals.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



