-
PDF
- Split View
-
Views
-
Cite
Cite
Dixon Osilli, Jelena Pavlovica, Rashi Mane, Mohammed Ibrahim, Amina Bouhelal, Sabu Jacob, Case reports: mild COVID-19 infection and acute arterial thrombosis, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa343, https://doi.org/10.1093/jscr/rjaa343
Close - Share Icon Share
Abstract
We present two cases of acute arterial thrombosis in patients who were confirmed to be SARS-CoV-2 positive. Neither of the patients had a background of underlying vascular morbidity. At the time of presentation, both patients exhibited only mild respiratory symptoms of COVID-19. After initial assessment and work-up, both patients underwent surgery for their respective vascular pathologies. They both did well post-operatively and were discharged home. This is an unusual presentation of acute arterial thrombosis in two patients with only mild symptoms of COVID-19 infection.
BACKGROUND
Coronaviruses are a large family of viruses which are important human and animal pathogens. In December 2019, a novel coronavirus was identified as the cause of viral pneumonia cases in Wuhan, a city in the Hubei Province of China. It rapidly spread, resulting in an epidemic throughout China, followed by an increasing number of cases worldwide. In February 2020, the World Health Organization designated the disease COVID-19, which stands for coronavirus disease 2019 [1].
Infection with COVID-19 primarily manifests with mild respiratory symptoms. In severe cases patients can progress rapidly and develop the acute respiratory distress syndrome, septic shock, metabolic acidosis and coagulopathy including a disseminated intravascular coagulation [2]. Understanding of COVID-19 is still evolving rapidly.
In this report, we describe two patients who presented with vascular complications (acute arterial thrombosis) in the background of COVID-19 infection.
CASE PRESENTATION
Case 1
A 60-year-old man presented to the emergency department with 1 day history of bilateral leg pain and a 2 day history of dry cough. The patient had a background of type II diabetes mellitus and hypertension.
On assessment, legs were painful, cold, pale and with partially reduced sensation and mobility. A Doppler probe confirmed absent lower limb pulses bilaterally from the common femoral arteries. An impression of acute aortoiliac occlusive disease was made.
Blood investigations showed an elevated white blood cell count (WCC), a low lymphocyte count and elevated C-reactive protein (CRP). The thrombin time was prolonged (Table 1). A computed tomography (CT)—angiogram of lower limbs showed complete thrombosis of the infrarenal aorta, the common and external iliac arteries bilaterally, the left common, proximal superficial and profunda femoral arteries (Fig. 1A). A CT scan of the chest showed patchy and ground-glass shadowing predominantly in the bilateral lower lung lobes (Fig. 1B). A throat swab was positive for COVID-19.
| . | Case 1 . | Case 2 . | Normal value . |
|---|---|---|---|
| FBC | (10 × 9 g/L) | ||
| WBC | 12.1 | 18.1 | 3.8–11 |
| PLT | 234 | 497 | 150–400 |
| Neutrophils | 10 | 15.8 | 2–7.5 |
| Lymphocytes | 1.1 | 0.9 | 1.5–4 |
| Clotting screen | (s) | ||
| PT | 11.4 | 14.6 | 9–13 |
| APTT | 26.3 | 26.1 | 20–33 |
| TT | 38.8 | 19.3 | 13–17 |
| Biochemistry | (mmol/L) | ||
| Na | 139 | 141 | 133–146 |
| K | 5.3 | 4.6 | 3.5–5.3 |
| Urea | 4.1 | 6.9 | 2.5–7.8 |
| Cr | 66 | 58 | 59–104 (umol/L) |
| CRP | 85 | 200 | 0–4.9 (ug/L) |
| . | Case 1 . | Case 2 . | Normal value . |
|---|---|---|---|
| FBC | (10 × 9 g/L) | ||
| WBC | 12.1 | 18.1 | 3.8–11 |
| PLT | 234 | 497 | 150–400 |
| Neutrophils | 10 | 15.8 | 2–7.5 |
| Lymphocytes | 1.1 | 0.9 | 1.5–4 |
| Clotting screen | (s) | ||
| PT | 11.4 | 14.6 | 9–13 |
| APTT | 26.3 | 26.1 | 20–33 |
| TT | 38.8 | 19.3 | 13–17 |
| Biochemistry | (mmol/L) | ||
| Na | 139 | 141 | 133–146 |
| K | 5.3 | 4.6 | 3.5–5.3 |
| Urea | 4.1 | 6.9 | 2.5–7.8 |
| Cr | 66 | 58 | 59–104 (umol/L) |
| CRP | 85 | 200 | 0–4.9 (ug/L) |
| . | Case 1 . | Case 2 . | Normal value . |
|---|---|---|---|
| FBC | (10 × 9 g/L) | ||
| WBC | 12.1 | 18.1 | 3.8–11 |
| PLT | 234 | 497 | 150–400 |
| Neutrophils | 10 | 15.8 | 2–7.5 |
| Lymphocytes | 1.1 | 0.9 | 1.5–4 |
| Clotting screen | (s) | ||
| PT | 11.4 | 14.6 | 9–13 |
| APTT | 26.3 | 26.1 | 20–33 |
| TT | 38.8 | 19.3 | 13–17 |
| Biochemistry | (mmol/L) | ||
| Na | 139 | 141 | 133–146 |
| K | 5.3 | 4.6 | 3.5–5.3 |
| Urea | 4.1 | 6.9 | 2.5–7.8 |
| Cr | 66 | 58 | 59–104 (umol/L) |
| CRP | 85 | 200 | 0–4.9 (ug/L) |
| . | Case 1 . | Case 2 . | Normal value . |
|---|---|---|---|
| FBC | (10 × 9 g/L) | ||
| WBC | 12.1 | 18.1 | 3.8–11 |
| PLT | 234 | 497 | 150–400 |
| Neutrophils | 10 | 15.8 | 2–7.5 |
| Lymphocytes | 1.1 | 0.9 | 1.5–4 |
| Clotting screen | (s) | ||
| PT | 11.4 | 14.6 | 9–13 |
| APTT | 26.3 | 26.1 | 20–33 |
| TT | 38.8 | 19.3 | 13–17 |
| Biochemistry | (mmol/L) | ||
| Na | 139 | 141 | 133–146 |
| K | 5.3 | 4.6 | 3.5–5.3 |
| Urea | 4.1 | 6.9 | 2.5–7.8 |
| Cr | 66 | 58 | 59–104 (umol/L) |
| CRP | 85 | 200 | 0–4.9 (ug/L) |

(A) A CT scan of the chest showed patchy and ground-glass shadowing predominantly in the bilateral lower lung lobes. (B) CT-thorax showing pulmonary changes. (C) CT-angiogram demonstrating aorta and left CIA patency with residual thrombus in right CIA post-operatively (blue arrow)
The patient had bilateral femoral thrombectomy. During the operation, a large amount of thrombus was removed from the abdominal aorta, both common iliac, external iliac and femoral arteries—allowing good flow to the left limb and fairly good flow to the right limb post-procedure.
A repeat CT-angiogram was performed. It confirmed that much of thrombus within the distal aorta and left common iliac arteries had been successfully removed; there was still a 25 mm occlusion in the proximal segment of the right common iliac artery with distal flow (Fig. 1C).
Case 2
A 75-year-old man presented with 2 days’ history of fatigue, malaise and non-productive cough with abdominal pain. He had a past medical history of diverticular disease and controlled hypertension.
Blood investigations showed an elevated WCC, a low lymphocyte count and elevated CRP. His prothrombin and thrombin times were also prolonged (Table 1). A CT scan demonstrated filling defects in the descending thoracic and abdominal aorta (Fig. 2A) and superior mesenteric artery (SMA) suggestive of acute thromboembolic phenomena. There was no sign of ischaemic bowel. A wedge-shaped peripheral hypodensity was seen at the mid-pole of the left kidney (likely to be a renal Infarct) (Fig. 2B). A CT of the chest showed patchy and ground-glass shadowing (Fig. 2C).
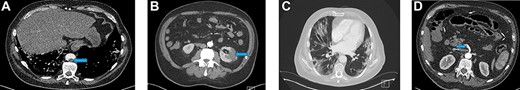
(A) Filling defect in aorta (blue arrow). (B) Left renal infarct (blue arrow). (C) CT-thorax showing pulmonary changes. (D) Thrombus in the distal SMA (blue arrow)
A COVID-19 swab at the time came back negative and it was not until later in the clinical course when subsequent swabs were reported positive.
The patient was initially treated conservatively with IV heparin infusion. However, in the 48 hours from the time of presentation, the patient developed increasing abdominal pain.
A repeat CT showed a SMA thrombus (Fig. 2D). Urgent angiogram and catheter-directed thrombolysis of the SMA was unsuccessful and the decision was made to operate. Exploratory laparotomy revealed a gangrenous segment of ileum necessitating resection of ~30 cm of small bowel. Re-look laparotomy at 48 hours showed no progression of ischaemia and thus anastomosis of the bowel ends was performed.
DISCUSSION
COVID-19 is caused by a betacoronavirus in the same subgenus as the severe acute respiratory syndrome (SARS) virus. The structure of the receptor-binding gene region is very similar to that of the SARS coronavirus, and the virus has been shown to use the same receptor, the angiotensin-converting enzyme 2 (ACE2), for cell entry [3]. It is notable that this receptor is widely distributed in body tissues and the vascular endothelium.
The most frequent serious presentation of covid-19 infection is pneumonia, manifested primarily with fatigue, dry cough, anorexia, myalgias and dyspnea [4]. Some patients do present with severe cardiovascular damage [5]. It is also known that patients with underlying cardiovascular diseases might have an increased mortality risk [6].
In COVID-19 patients, some of the typical laboratory findings include lymphopaenia, raised lactate dehydrogenase levels, raised liver transaminase levels, and raised inflammatory markers (e.g. CRP, ferritin and erythrocyte sedimentation rate) [7, 8]. The most common haemostatic abnormalities in these patients include a mild thromobocytopaenia, elevated D-dimer levels and elevated prothrombin time [9]. Some of these laboratory features have been associated with worse outcomes [10]. It is unknown whether the haemostatic abnormalities seen in COVID-19 patients are due to a specific effect of the virus or due to a cytokine storm associated with the systemic inflammatory response as seen in other viral infections [11].
Direct data on the thromboembolic risk with COVID-19 are limited. Most of the evidence linking COVID-19 infection to a higher risk of thromboembolism has focused on hospitalized, critically ill patients. A number of authors have noted the high proportion of aberrant coagulation in this cohort with severe disease. Both patients in this report were not critically ill at the time of presentation.
It is unknown whether infection with COVID-19 does exacerbate the development of acute arterial thrombosis in the setting of underlying atherosclerosis. Anecdotal evidence also suggests the occurrence of microvascular thrombosis, although concrete data from published studies have not reported an increased incidence of large vessel thrombosis (VTE) (e.g., lower extremity deep venous thrombosis or pulmonary embolism). One small Chinese case series suggested benefit from anticoagulation in patients with a high sepsis-induced coagulation score and elevated D-dimer >6 times the upper limit of normal [12].
The role that the ACE2 receptor plays in contributing to the haemostatic abnormalities seen in SARS-CoV-2 infection remains to be fully elucidated. It is unknown whether SARS-CoV-2 can lead to abnormal coagulation by invading vascular endothelial cells expressing high levels of ACE2 [13]—particularly in those patients with mild disease.
CONCLUSION
Although the general condition of COVID-19 patients may predispose to venous and arterial thromboembolism due to an increased inflammatory response, the exact mechanism is still unclear.
In COVID-19 patients, even in those with mild disease, a high index of suspicion should be maintained for serious thromboembolic events and further data regarding the impact of the thrombotic risk and the impact of VTE prophylaxis or anticoagulation in COVID-19 patients are needed.



