-
PDF
- Split View
-
Views
-
Cite
Cite
Mariam Rela, Giles Bantick, Fibro-osseous pseudotumour of the digit—a diagnostic challenge, Journal of Surgical Case Reports, Volume 2020, Issue 5, May 2020, rjaa125, https://doi.org/10.1093/jscr/rjaa125
Close - Share Icon Share
Abstract
A 60-year-old right-hand dominant woman presented to the emergency department with a 3-week history of pain and swelling in her right thumb. The X-ray showed evidence of erosion at the tip of the distal phalanx. Her initial management included surgical debridement with bone biopsies and intravenous antibiotics. The initial working diagnosis was a soft tissue infection of the thumb tip, causing osteomyelitis of the distal phalanx. The X-ray findings also raised the suspicion of a possible bone tumour. She was treated as having osteomyelitis and attended ambulatory care for daily intravenous antibiotics for 2 weeks. Initial histology was reported as a spindle cell tumour; however, following discussion at the sarcoma MDT, a diagnosis of a fibro-osseous pseudotumour of the digit was made. This is a benign lesion that was managed non-operatively in this patient. This case emphasises the importance of considering all differential diagnoses, even in a common presentation.
INTRODUCTION
Whilst this case represents a common presentation, it presented a diagnostic challenge. It highlights the importance of considering all of the options in a differential diagnosis whilst not delaying the treatment. The possibility of a patient presenting with what seemed like a simple infection of the thumb having an underlying malignant bone tumour was surprising and enlightening. It made the healthcare professionals involved reflect on all of these cases to ensure potentially serious diagnoses are not missed. This case also highlights effective communication with the patient given an uncertain diagnosis. Furthermore, input from multidisciplinary teams including plastic surgery, radiology, histopathology and microbiology allowed a consensus to be reached and for the best management for the patient to be carried out.
CASE REPORT
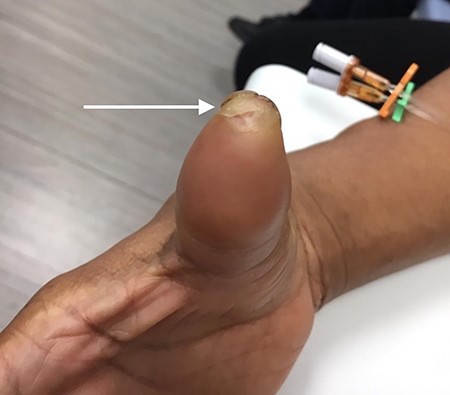
A 60-year-old right-hand dominant cleaner presented to the emergency department with a 3-week history of pain and swelling in her right thumb tip. She was a Colombian female with a past medical history of hypothyroidism on thyroxine replacement and was a non-smoker who was independent of activities of daily living. She reported her right thumbnail had always grown with a vertical split in the midline (Fig. 1) and felt her symptoms began after trimming this nail. She had completed a course of oral flucloxacillin from her GP 5 days previously with no improvement in her symptoms. On examination, her right thumb was swollen (Fig. 2) with tenderness under the nail plate, no pulp tenderness and no erythema or obvious collection. There was a small area of peeled, dead skin at the tip of the thumb (Fig. 3), but the digit was neurovascularly intact. There was no evidence of flexor sheath infection on presentation as she had no Kanavel signs.

Right thumb with vertical split at the distal end of the nail plate.

Her blood tests on presentation were unremarkable and X-rays of her right thumb showed a lytic lesion involving the tuft of the distal phalanx (Figs. 4 and 5). She was admitted to the hospital and was treated as having an infection of her right thumb with elevation and intravenous antibiotics. She underwent emergency surgery the next day for a washout and debridement of the right thumb. During the debridement in theatre, there was no pus in the pulp, but the bone was found to be eroded and soft, thus multiple specimens from the bone were sent for microscopy, culture and sensitivity, acid-fast bacilli (AFB) and histopathology.

AP radiograph of right thumb showing erosion of tip of distal phalanx.

Lateral X-ray of right thumb showing erosion of tip of distal phalanx and soft tissue swelling.
She was discharged 2 days later, with a decision to continue daily intravenous antibiotics in ambulatory care to treat the osteomyelitis. Citrobacter freundii was isolated from the bone biopsies on enrichment culture, and the AFB culture was found to be negative. Microbiology advised continuing with 6 weeks of intravenous antibiotics.
The initial histopathology report was released 2 weeks after the biopsies were sent and described fragments of a cellular spindle cell tumour with islands of osteoid, which was suspicious for a primary bone malignancy. This triggered the pathway for suspected primary bone malignancy, with the histopathology specimen being sent to a sarcoma unit for specialist reporting and the patient being referred to the sarcoma multidisciplinary team meeting (MDT).
Following this, the patient was reviewed in clinic having completed 2 weeks of intravenous antibiotics and showed no signs of ongoing infection; thus, antibiotics were discontinued. Importantly, the patient was kept up-to-date throughout these investigations. It was explained to her that there was a possibility of her having a malignant bone tumour, which would likely require specialist treatment. She would have likely required amputation and adjuvant chemotherapy, which could have had serious consequences for her ability to work.
The outcome from the sarcoma MDT delineated that the histopathology showed a myofibroblastic tumour best classified within the nodular fasciitis spectrum of lesions. Its conclusion, taking into account the imaging, was that the morphological features were most in keeping with a fibro-osseous pseudotumour of the digit with no evidence of malignancy, possibly in association with infection.
The patient was then reviewed 6 weeks after her initial presentation, following the results of the sarcoma MDT, which confirmed a benign tumour. At this point, the patient reported some tenderness around the surgical incision, but that her symptoms were improving. It was thought that she had no signs of ongoing infection in the thumb. The outcome was for monitoring of her symptoms with no indication for surgical excision. She had a follow-up X-ray in 6 weeks’ time that showed resolution of the lytic lesion (Figs 6 and 7).

AP follow-up radiograph of right thumb 6 weeks post-admission showing resolution of lytic lesion.

Lateral follow-up radiograph of right thumb 6 weeks post-admission showing resolution of lytic lesion.
DISCUSSION
There have been few published cases of fibro-osseous pseudotumours of the digit. This diagnosis was first described by Dupree and Enzinger in 1986 as consisting of ‘benign fibroblastic proliferations with foci of osseous differentiation in digits’ [1]. The most common presentation is of a painful, erythematous, localised swelling of the digit [2], which occurs most frequently in young to middle-aged women [3]. In a recent study, there was an association with antecedent trauma and occupations involving repetitive manual labour [4]. Both of these positive associations correspond to this patient. Histologically, these lesions consist mainly of ‘well-differentiated spindle cells with mature and immature fibroblastic foci and associated osteoid formation’ [2], which is almost exactly what was reported in this case initially. Given the unusual histological features of this condition, it is commonly mistaken as a malignant lesion [2]; such as a periosteal osteosarcoma. The treatment is the complete excision of the lesion. Prognosis following removal is excellent, with no tendency towards recurrence and no reported cases of malignant transformation [3]. In this case, excision was not performed as the patient’s symptoms were resolving and the risks outweighed the benefits.
The initial diagnosis in our patient was of a soft tissue infection. Due to the pulp of the fingertip being divided by a number of fibrous septa running from the skin to the periosteum, there is a risk of infection spreading to the bone, resulting in osteomyelitis [5]. Additional sequelae of this serious infection include fingertip compartment syndrome, digital tip necrosis and flexor tenosynovitis [6]. Hence, prompt management as above given the suspicion of infection was necessary to prevent the aforementioned complications.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



