-
PDF
- Split View
-
Views
-
Cite
Cite
Ammar Al-Najjar, Julien Al Shakarchi, Melwyn Pereira, Richard Downing, An unusual presentation of acute onset Charcot arthropathy, Journal of Surgical Case Reports, Volume 2020, Issue 5, May 2020, rjaa128, https://doi.org/10.1093/jscr/rjaa128
Close - Share Icon Share
Abstract
Charcot arthropathy is a progressive condition primarily affecting the lower limbs in patients with diabetes mellitus. It is a rare complication of diabetic neuropathy and if left untreated can lead to severe limb destruction necessitating major amputation. Here, we report the case of a 41-year-old female who presented with rapidly progressive Charcot foot over a 10-day period, necessitating open reduction and internal fixation of Lisfranc-type fracture dislocations. Her presentation with a rapidly progressing red, swollen foot with a blister on the plantar aspect prompted initial treatment on the basis of a diabetic foot infection. The report will therefore serve as a useful reminder to maintain a high index of suspicion for Charcot foot, which may present in an atypical manner.
INTRODUCTION
Charcot neuroarthropathy (also known as Charcot arthropathy/Charcot foot) is a rare but serious complication of diabetic peripheral neuropathy [1] affecting 0.15–2.5% of diabetic patients [2]. The consequences of misdiagnosis or of failing to treat the condition can be devastating, leading to major amputations and limb loss. Whilst the exact pathophysiology of Charcot foot remains debated, a multifactorial pathogenesis involving neurological and vascular changes in the insensate foot seem likely, with neurovascular and neurotraumatic theories predominating [3]. Cases typically present with a history of trauma, demonstrating considerable unilateral swelling, erythema and localized increase in temperature to the foot, with intact skin. In advanced cases with considerable mid-foot destruction, a typical ‘rocker bottom’ appearance is seen [2]. In most cases, progression of deformity takes a more chronic form and is seen over a period of months, to years [4].
This case report describes a case of very rapidly destructive Charcot foot with plantar blistering over a short time frame, which was initially managed as a case of diabetic foot infection.

Initial foot X-rays (AP and lateral views), exhibiting normal appearances.
CASE REPORT
A 41-year-old female, with a background of Type 1 Diabetes Mellitus (T1DM), previous diabetic foot infection and peripheral neuropathy, presented acutely with a hot, swollen and erythematous left foot. Ten days prior, she sustained a fall whilst walking. The patient denied injury, swelling or pain at the time, though she presented to the emergency department (ED) 2 days following the fall with a new-onset foot swelling. Initial imaging with plain film X-ray, as well as blood tests, was unremarkable (Fig. 1), and she was discharged from the ED. A plantar blister appeared over the following days, with subsequent worsening of foot swelling and erythema over a 10-day period, culminating in her acute presentation (Fig. 2).

Examination revealed a warm, swollen and mildly erythematous left foot, with a localized blister to the plantar aspect. Blood tests showed an elevated C-reactive protein (CRP 65), normal white cell count and a thrombocytosis (platelet count 635). This was initially managed as diabetic foot infection with intravenous antibiotics and offloading, given the rapid speed of onset and progression, with a clinical picture of cellulitis and a localized blister.
At this presentation, plain film X-ray revealed complete fracture dislocations of the second to fifth tarsometatarsal joints, involving the lateral, middle and medial cuneiform bones of the left mid-foot (Lisfranc fracture dislocations; Fig. 3). This was correlated with bone CT (computed tomography) and MR (magnetic resonance) imaging, with interval changes noted to be of rapid onset (Fig. 4).

Foot X-rays taken at acute presentation (AP and lateral views), demonstrating rapid interval progression and destruction to mid-foot.
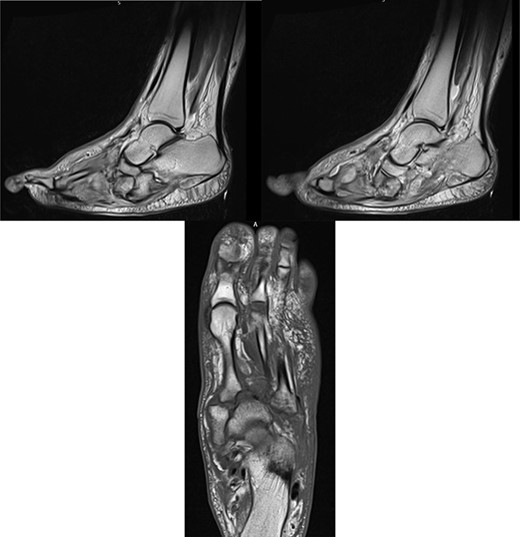
MR images, correlating plain film findings of acute mid-foot destructive changes; typical ‘rocker bottom’ appearance of plantar aspect of foot is seen.
DISCUSSION
Though rare, Charcot foot is a recognized, well-documented complication of diabetic neuropathy. The mechanism by which this occurs is not fully understood, but two theories exist—namely, the neurovascular and neurotraumatic theories [5]. In the neurovascular theory, an underlying autonomic neuropathy leads to hypervascularity, osteolytic change and demineralization. However, the neurotraumatic hypothesis postulates that unperceived trauma to an insensate extremity leads to continued bony destruction on ambulation, which worsens and progresses. These theories imply that a sufficient time frame is required for established Charcot foot destruction to develop.
Cases of acute progression over weeks have been reported in the literature [6], with the typical progression occurring over months to years [1, 4]. However, to the best of our knowledge, the progression seen in our patient, from normal X-ray appearances to established, acute Charcot foot with considerable mid-foot destruction over a period of just 10 days, has not been previously described in the literature. Ultimately, there was minimal delay in subsequent correct diagnosis and management. The combination of a blister, erythema, cellulitis, rapid progression and elevated inflammatory markers led to initial clinical suspicion of diabetic foot infection, but a lack of response to intravenous antibiotics raised the suspicion of acute Charcot foot.
As acute Charcot foot is managed by primary fixation, early recognition is critical to ensure improved outcomes. A through neurological exam revealing features of diabetic neuropathy is vital, as a common prerequisite for acute Charcot foot. Differentiation between acute Charcot foot and infection clinically could also be achieved by elevating the affected limb, observing a decrease in localized oedema/swelling in a Charcot picture [7, 8]. Additionally, the presence of ulcers should raise the suspicion of infection or osteomyelitis, and therefore, the importance of early imaging cannot be overstated. Modestly raised inflammatory markers (as demonstrated in the case) are more likely to suggest

Post-operative X-rays (AP and lateral), demonstrating good reduction and fixation of fracture dislocations.
an acute Charcot foot than an infectious process, the latter frequently presenting with higher laboratory values [8, 9].
The patient was initially managed with a total contact leg cast, followed by open reduction and internal fixation (ORIF) with locking plates, combined with lengthening of the tendo-Achilles to permit full dorsiflexion and subsequent re-casting (Fig. 5). Her post-operative progress was satisfactory, and she is currently non-weight bearing for 6 months post-ORIF.
The case highlights the importance of a high index of suspicion for Charcot foot, when a patient presents with a unilaterally swollen, erythematous and warm extremity with a history of trauma, however recent. We hope it will serve as a useful reminder to clinicians when dealing with such presentations.
References



