-
PDF
- Split View
-
Views
-
Cite
Cite
Jonathon Kyriakides, Ashlyn Stackhouse, Vomiting-induced pneumomediastinum as a result of recurrent Boerhaave’s syndrome, Journal of Surgical Case Reports, Volume 2020, Issue 5, May 2020, rjaa102, https://doi.org/10.1093/jscr/rjaa102
Close - Share Icon Share
Abstract
Vomiting-induced pneumomediastinum can be a result of barotrauma causing alveolar rupture or Boerhaave’s syndrome. Although a rare cause of secondary pneumomediastinum, Boerhaave’s syndrome allows extravasation of air and fluid due to oesophageal perforation. We report a case of a 20-year-old female who presented with prolonged vomiting during a panic attack. Extensive surgical emphysema and pneumomediastinum were visualised radiologically. A source of oesophageal rupture was not visualised on cross-sectional computed tomography imaging following contrast ingestion. A complication of mediastinitis provided the evidence that this was a case of Boerhaave’s syndrome whereby microscopic perforation of the oesophagus led to secondary pneumomediastinum, rather than vomiting-induced spontaneous pneumomediastinum caused by barotrauma. Recurrent Boerhaave’s syndrome in this case is owed to the patient having previously experienced identical symptoms which spontaneously resolved.
INTRODUCTION
Surgical emphysema and pneumomediastinum often occur in conjunction due to a communication via fascial planes. Pneumomediastinum is classed spontaneous when there is no identifiable cause or trauma. In contrast, secondary pneumomediastinum has an identifiable cause.
Boerhaave’s syndrome is an uncommon yet recognised precipitant of secondary pneumomediastinum. It occurs following oesophageal rupture during forceful vomiting or retching. Although oesophageal rupture is itself a rare occurrence, there are even fewer cases of recurrent Boerhaave’s syndrome [1].
Vomiting-induced pneumomediastinum without the evidence of oesophageal perforation is often described as a spontaneous pneumomediastinum. We present a case of vomiting-induced pneumomediastinum, where no source of viscous perforation or airway injury was identified. We review the literature and explain why our case is one of recurrent Boerhaave’s syndrome causing secondary pneumomediastinum but without an identified oesophageal perforation, for which it is unique.
CASE REPORT
A 20-year-old female patient presented to the emergency department with a severe anxiety attack lasting 7 days. She reported chest and throat tightness, vomiting and dry retching, and crepitus on palpation of her neck. An undiagnosed anxiety disorder was her only medical history of note. She reported similar crepitus in her neck following an anxiety attack some months previously, which resolved.
On initial assessment, pneumoderma was palpable on the anterior chest wall and neck. Blood tests revealed a haemoglobin level of 176 g/L (normal range 110–150 g/L) and white blood cell count of 17.71 × 109/L (normal range 3.5–11 × 109/L). Serum urea and creatinine were mildly raised from her baseline. The C-reactive protein level was 7 mg/L (normal range < 5 mg/L). These results were largely explained by dehydration secondary to prolonged vomiting. A chest radiograph (Fig. 1) revealed extensive surgical emphysema and pneumomediastinum.
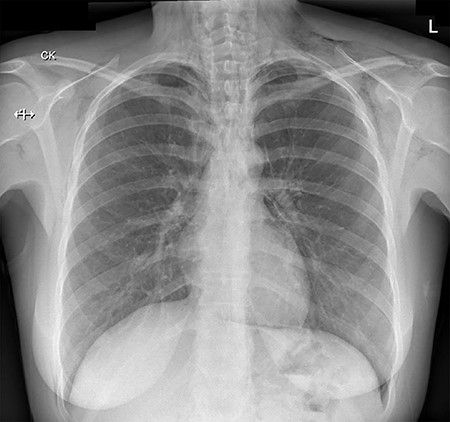
A chest radiograph illustrating surgical emphysema and pneumomediastinum.
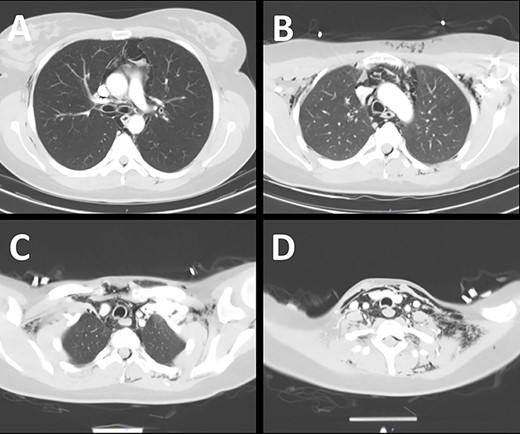
An enhanced CT scan of the neck and chest demonstrating extensive surgical emphysema and pneumomediastinum.
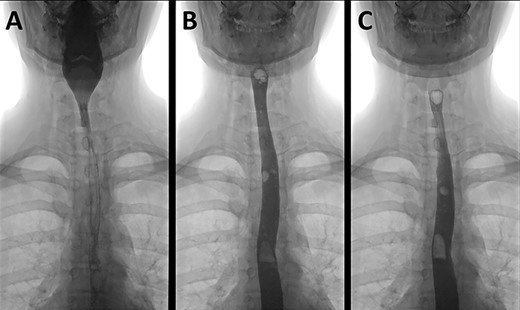
A water-soluble contrast swallow examination demonstrating contrast passing from the pharynx (A) through the oesophagus (B and C) with no evidence of leak.
An enhanced computed tomography (CT) scan of the neck and chest is shown in Fig. 2. This demonstrated extensive pneumomediastinum (A), as well as subcutaneous emphysema extending from the chest wall (B) into the soft tissues of the neck (C and D). Air was noted to have leaked into the spinal canal. Imaging did not reveal a tracheal tear or airway injury.
Nasendoscopy to the level of the vocal cords did not reveal an obvious source of air leak. Neither an enhanced CT thorax and abdomen following oral gastrograffin contrast, nor a water-soluble contrast swallow examination (Fig. 3) showed any evidence of contrast leak or identify a source of perforation.
The patient was commenced on antibiotics, intravenous fluids and kept nil by mouth. During the initial observation period, a clinical diagnosis of mediastinitis was made due to worsening chest pain, fevers and rising inflammatory markers. Broad spectrum antibiotics were continued. A normal diet was re-introduced 8 days post-presentation. A chest radiograph performed 2 weeks post-discharge demonstrated complete resolution of pneumomediastinum and surgical emphysema.
DISCUSSION
Spontaneous pneumomediastinum results from alveolar rupture rather than gastrointestinal leak. It occurs due to bronchial hyper-reactivity or barotrauma; the latter of which can be induced by coughing or vomiting. Alveolar rupture allows air to be drawn into the mediastinum down a pressure gradient.
Several case reports suggest that vomiting-induced pneumomediastinum does not always indicate oesophageal rupture, explained by barotrauma secondary to vomiting [2–4]. In these case reports, oesophageal rupture was not identified on imaging.
Mediastinitis is usually a consequence of oesophageal perforation or iatrogenic causes. Mediastinitis can occur following secondary pneumomediastinum, but is not typically seen following spontaneous pneumomediastinum [5]. This is supported by Ebina et al. [6], who reviewed 34 cases of spontaneous pneumomediastinum and found that none developed mediastinitis. A diagnosis of mediastinitis in our case, together with the absence of neither reparatory disease nor smoking history, makes vomiting-induced spontaneous pneumomediastinum unlikely.
Oesophageal rupture, or Boerhaave’s syndrome, occurs due to a sudden increase in intra-oesophageal pressure from vomiting against a closed glottis. The resultant transmural tear allows air and free fluid to leak out of the oesophagus. This oesophageal tear usually occurs in the lower third of the oesophagus, due to an inherent weakness in connective tissue between muscular fibres in this area [7]. Complications depend on the exact location of the oesophageal tear: distal oesophageal tears usually result in a left hydropneumothorax, whilst mid-oesophageal tears usually result in a right pneumothorax [8]. The investigation of choice for Boerhaave’s syndrome is an enhanced CT scan following oral contrast, allowing extravasation of contrast to be identified.
We hypothesise that our case of vomiting-induced pneumomediastinum is a result of Boerhaave’s syndrome whereby microscopic oesophageal perforation allowed extravasation of air over a period of time, exacerbated by each episode of vomiting. Microscopic perforation would explain why contrast leak was not identified on imaging.
Our patient described similar crepitus in her neck after prolonged vomiting some months prior, which spontaneously resolved. Hence, this is likely a case of recurrent Boerhaave’s syndrome. Recurrent Boerhaave’s syndrome is a rare phenomenon, with only eight cases described in the literature [1]. An inherent anatomical abnormality in the oesophagus or a temporary oesophagitis are likely to explain recurrent Boerhaave’s syndrome, due to such few cases being described yet the incidence of severe vomiting being relatively high [1].
In conclusion, our case is unique in that it describes recurrent Boerhaave’s syndrome causing secondary pneumomediastinum via an oesophageal perforation not visible on cross-sectional imaging. This differs from vomiting-induced spontaneous pneumomediastinum. Conservative management to allow microscopic oesophageal perforation to heal results in clinical and radiological resolution of pneumomediastinum. This reiterates the importance of admission for observation and administration of antibiotics in cases of vomiting-induced pneumomediastinum to prevent potentially life-threatening complications of Boerhaave’s syndrome.
CONFLICT OF INTEREST STATEMENT
None declared.



