-
PDF
- Split View
-
Views
-
Cite
Cite
Nikhil Sahdev, Karan Punjabi, Luke Williams, Adam Peryt, Aman Coonar, Giuseppe Aresu, Uniportal subxiphoid bilateral removal of self-introduced thoracic foreign bodies, Journal of Surgical Case Reports, Volume 2020, Issue 4, April 2020, rjaa052, https://doi.org/10.1093/jscr/rjaa052
Close - Share Icon Share
Abstract
This is a report of a 31-year-old male refugee, who was admitted to Intensive Therapy Unit after being found in severe chest pain after escaping extreme torture from his home country. He was found to have four nails in his thorax. These were removed using a subxiphoid video-assisted thorascopic surgery (VATS) technique. This technique allowed excellent visualization of the right, left and anterior mediastinal part of the chest and therefore preventing damage or injury to surrounding structures. This was particularly useful in a complex case such as this. By avoiding an intercoastal incision and intercostal manipulation, our patient had limited pain post-procedure facilitating an earlier aggressive mobilization program with potential benefit in terms of improved lung expansion, reduction of atelectasis and lung infections. With the right training, the technical challenges of using the technique should be overcome and thus the benefits of subxiphoid VATS will be offered to a larger portion of thoracic surgical patients.
INTRODUCTION
Uniportal video-assisted thorascopic surgery (VATS) has become an increasingly used technique for minimally invasive thoracic surgery over the previous few years [1]. Traditionally in thorascopic surgery, 2–4 operating ports are placed in the lateral chest wall increasing the possibility of postoperative chronic pain and chest wall numbness. Uniportal VATS uses a single port with potential benefits related to the fact that only one intercoastal space is involved [1]. Further advances in surgical techniques, camera technology and surgical instrument design have allowed the uniportal approach to become a more viable technique for an increased number of procedures [1].
The subxiphoid VATS approach has been introduced with the aim to further reduce the surgical stress and postoperative acute and chronic pain and overall quality of life, as there is no injury of the intercostal nerves. The reduction of the surgical trauma is even more important in bilateral procedures as both chest cavities can be reached from a single subxiphoid incision.
The subxiphoid approach has been used for many different procedures including anatomical and non-anatomical lung-resections, resection of mediastinal masses and thymectomy in myasthenic patients.
We present the case of a 31-year-old male who underwent removal of four nails in the thorax via a uniportal subxiphoid VATS approach.
CASE REPORT
This is a report of a 31-year-old male refugee with a history of psychiatric problems, who was admitted to the Intensive Therapy Unit after being found on a motorway. He was in severe chest pain after escaping extreme torture from his home country. On examination, he found to have a nail (Nail 1) penetrating the anterior chest wall (Fig. 1). On further imaging (Fig. 2), he had three further nails in his thorax (Nail 2: right upper lobe, Nail 3: right lower lobe, Nail 4: left upper lobe).

Image of Nail 1: externally visible penetrating anterior chest wall.
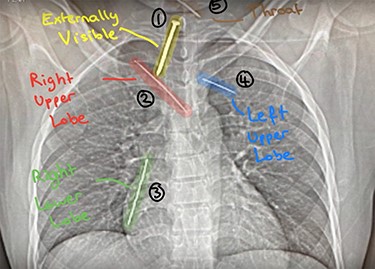
Chest X-ray: detailing the position of four nails within the thorax (Nail 2: right upper lobe; Nail 3: right lower lobe; Nail 4: left upper lobe) and Nail 5 (throat).
THE PROCEDURE
Nail 1 (externally visible) was superficially removed using a grasper.
In order to remove Nails 2–4, a subxiphoid VATS approach was considered safer and less invasive as it allows an excellent visualization of both pleural cavities using a single, muscle and intercostal nerves sparing procedure.
The operation was conducted with the patient lying in a supine position. A single incision was made distally to the xiphisternum, the dissection was then carried out along the linea alba to reach the anterior mediastinum posteriorly to the sternum. The sternum was then lifted using a Rultract® Skyhook Retractor to improve both the exposure of the pleural cavities and the working space (Fig. 3). To further increase the working space double tube ventilation was used. When operating on the right chest cavity, we excluded the ventilation of the right lung and vice versa for when working on the left lung. A 30° 10 mm diameter scope was used to visualize the pleural cavities.
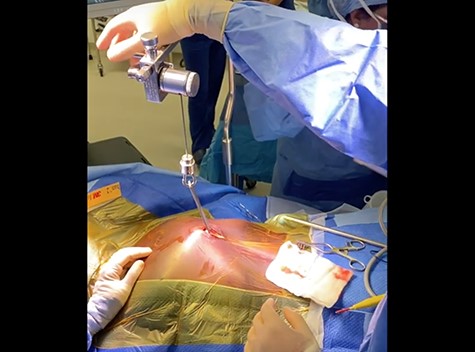
Image showing the sternum being lifted using a Rultract® Skyhook Retractor to allow good access to the pleural cavities.
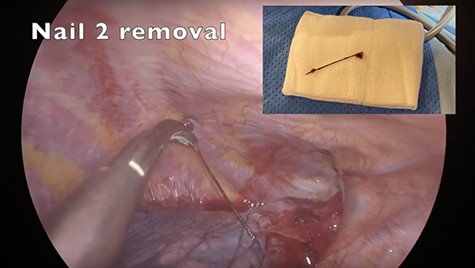
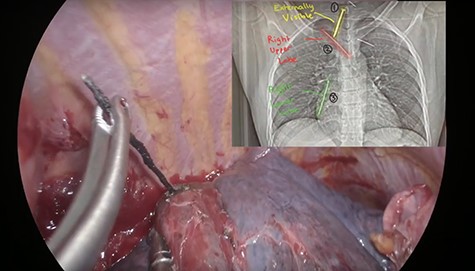
First the right pleural cavity was entered. Using an energy device LigaSure™ Maryland Jaw Thoracic Sealer36cm Nail 2 was exposed in the right upper lobe and removed (Fig. 4). Nail 3 in the right lower lobe was particularly difficult to expose; however, by thorough instrumental palpation, it was eventually located and, using diathermy, an incision was made at the level of the surface of the lung, and it was exposed and removed (Fig. 5). To locate Nail 4 in the left upper lobe the anaesthetist was asked to stop ventilating the left lung. Using a similar technique of instrumental palpation, Nail 4 was identified and then removed (Fig. 6). After the operation was complete, the single wound was closed, and a single chest drain was inserted (Fig. 7).


DISCUSSION
Transthoracic VATS with 2–3 incisions is routinely used for various thoracic diseases. This technique has already been shown to reduce postoperative pain and shorten hospital stays compared to open procedures [2]. Following this uniport VATS has shown to reduce the overall rate of complications, length of hospital stay and duration of postoperative drainage even further, yet chest trauma still remains an issue [3, 4]. However, by using subxiphoid approach trauma and compression to the intercoastal nerves (which is often the major source of postoperative pain and paraesthesia) can be completely avoided.
The subxiphoid VATS procedure is now beginning to be used for a variety of procedures including resection of thymomas, bilateral spontaneous pneumothorax and pulmonary lobectomies [5–7].
The subxiphoid VATS technique has many benefits. One of these includes no reduction in shoulder movement after surgery due to the integrity of the thoracic cavity being maintained [8]. The technique also allows both pleural cavities to be accessed in a single operation, particularly useful in bilateral pulmonectomies. Some surgeons may agree that the angle at which the staplers are introduced may be even more convenient than the intercostal approach to the upper and middle lobes. Cosmetically there is also a clear advantage as there is minimal scaring post-operation.
In this particular case, subxiphoid VATS was used as it allowed excellent visualization of the right, left and anterior mediastinal part of the chest, including the phrenic nerves preventing damage or injury to surrounding structures. This was particularly useful in a complex case such as this. By avoiding an intercoastal incision and intercostal manipulation, our patient had limited pain post-procedure and allowed earlier aggressive mobilization.
Some drawbacks of the technique include compression of the heart and arrhythmia in left sided operations. The key is continuous and comprehensive monitoring for circulatory disturbance and arrhythmia intraoperatively. Should arrhythmia develop it is important that it is managed rapidly and effectively in such a manner to minimize haemodynamic disturbance [9]. Sometimes in technical difficultly or excessive bleeding the surgeon may wish to convert to an intercostal approach. However, with improved handling skills and experience the incidence of accidental intraoperative bleeding should decrease [10].
The benefits of reduced postoperative pain, excellent visualization of structures and minimal scaring are making the subxiphoid approach attracting to an increasing number of surgeons. With the right training and experience the subxiphoid technique could be used to perform in a safe way an increasing number of operations including bilateral procedures like the one that we have described with potential benefit for patients.
ACKNOWLEDGMENTS
The authors have nothing to declare.
DISCLOSURES
None
References
Author notes
Nikhil Sahdev and Karan Punjabi are joint first authors.



