-
PDF
- Split View
-
Views
-
Cite
Cite
Tomoya Iwaasa, Keiji Tensho, Suguru Koyama, Hiroki Shimodaira, Hiroshi Horiuchi, Naoto Saito, Jun Takahashi, Plica syndrome after medial patellofemoral ligament reconstruction: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 4, April 2020, rjaa036, https://doi.org/10.1093/jscr/rjaa036
Close - Share Icon Share
Abstract
A 16-year-old female with a history of left recurrent patellar dislocation underwent medial patellofemoral ligament (MPFL) reconstruction surgery. Two months postoperatively, the patient presented with medial patellar pain. Left medial plica syndrome was suspected, and we performed a partial arthroscopic resection of the medial synovial plica. The symptom gradually improved after surgery. To the best of our knowledge, there are no reports that discuss the relationship between postoperative pain of MPFL reconstruction and synovial plica as found in this case report. Surgeons should be aware of the possibility that asymptomatic synovial plica could become symptomatic.
INTRODUCTION
Medial patellofemoral ligament (MPFL) reconstruction has been reported as a widely used treatment of recurrent patellar dislocation due to its good mid-to-long term outcomes [1, 2]. However, complications such as patellar instability, re-dislocation, patellar fractures and postoperative pain have also been reported [3]. Although various sources of postoperative pain have been reported in the literature, we report a case of knee pain following MPFL reconstruction that was thought to be caused by medial plica syndrome, which exhibited improved symptoms after the removal of synovial plica.
CASE REPORT
A 16-year-old female with a history of recurrent patellar dislocation underwent MPFL reconstruction surgery (Fig. 1). There was no pain nor tenderness in the medial patella, and the apprehension test was positive before surgery. Preoperative magnetic resonance imaging (MRI) showed no injury to the cartilage in the patellofemoral (PF) joint, and hypertrophic medial plica was observed. Arthroscopy showed no cartilage injury in the PF joint. For the tendon graft, a tape-type artificial ligament with a width of 15 mm (Leeds-Keio Ligament, Xiros plc, Leeds, United Kingdom) was used [2]. A bone tunnel was constructed to pass the ligament through the medial side and anterior surface of the patella, and the folded ligament was pulled into the femoral tunnel and fixed at 60° flexion with a bioabsorbable screw (BIOSURE PK Screw, Smith & Nephew Inc., Endoscopy Division, Mansfield, MA, United States). The tension pattern of the reconstructed ligament exhibited laxity under flexion and mild tension under extension. ROM exercises and partial weight-bearing were allowed at 1 week postoperatively and gradually progressed to full weight-bearing at 4 weeks postoperatively.

Radiographs of the left knee after MPFL reconstruction. Anteroposterior (A), lateral (B) and axial (C) radiographs of the left knee after MPFL reconstruction showing the entry of patella tunnel (white arrow), entry of femoral tunnel (white dot arrow) and bone tunnel of patella (white dot line). Patella tilt of post-operation was similar to that of pre-operation.
Two months postoperatively, the patient presented with the pain in the medial margin of the patella during walking and knee extension, and the pain continued when she was allowed to start rhythmic gymnastics at 6 months postoperatively. There was no evidence of swelling, crepitus and ROM restriction, and her apprehension sign was also negative. Pain was relieved by an intra-articular xylocaine injection. Postoperative MRI showed no clear injury to the cartilage of the medial PF joint, and the medial PF joint space and the size of the medial plica were almost the same as before surgery (Fig. 2). Based on these findings, left medial plica syndrome was suspected. Although the patient underwent conservative treatment consisting of analgesics and physiotherapy, there were no signs of improvement, and consent was obtained for undergoing arthroscopic surgery at 8 months after the initial surgery. Intraoperative arthroscopic findings with probing confirmed an unenlarged but hardened and thickened medial plica (Fig. 3). No injury to the patellar and femoral cartilage was observed. The synovial plica was considered the main cause of pain, and we performed a partial resection of the medial synovial plica. The pain and the tenderness at the medial margin of the patellar during walking and exercising had gradually improved after surgery. The Lysholm scale improved from 85 to 100 points. At 2 years postoperatively, the patient has currently no pain in the medial side of the patella, negative apprehension sign. She has returned to play in rhythmic gymnastics.
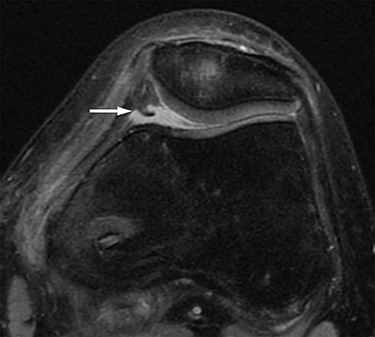
MRI. Axial proton density-weighted (TR = 3000, TE = 12) image before medial patellofemoral ligament (MPFL) reconstruction revealing medial synovial plica (white arrow). The medial patellofemoral joint space and the size of the medial plica after MPFL reconstruction are almost the same as before surgery. There are no clear signs of injury to the cartilage in the patellofemoral joint.
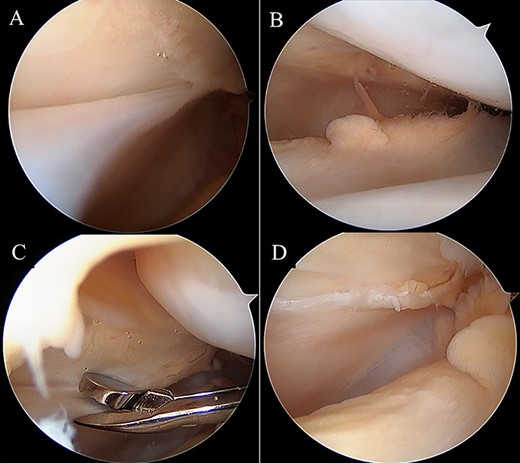
Intraoperative arthroscopic views. Medial synovial plica with a tight and hypertrophic margin (A). No injury to the patellar and femoral cartilage was observed (B). The synovial plica was partially removed with oval forceps (C). Image after removal (D).
DISCUSSION
Various causes have been reported for postoperative pain after MPFL reconstruction, to the best of our knowledge, for example, implant-related stimulation, cartilage injury to the patella or femoral trochlea, a tight MPFL reconstruction graft, remaining of patella instability and scar tissue [3, 4]. But there are no reports that discuss the relationship between postoperative pain and synovial plica as found in this case report.
In the present case, there was neither pain nor tenderness at the site of fixation, so we concluded that implant-related stimulation is not its cause of the postoperative pain. Moreover, there was no observable cartilage injury to the patella or femoral trochlea, and there was no fibrous scar tissue under arthroscopy during re-operative surgery; thus, they were ruled out as causes of the pain. Her apprehension sign was negative, and we did not add any operative procedure for reconstructed MPFL ligament, so looseness or tightness of the graft was ruled out too. We determined that the postoperative pain was caused by plica syndrome because we confirmed a medial synovial plica on preoperative MRI in addition to pain in the medial side of the patella and the symptoms improved after the surgical removal of plica.
Medial plica is a synovial fold that is located in the medial wall of the joint, wherein many are asymptomatic normal structures [5]. In the present case, the primary reason that the medial synovial plica that was native to the patient prior to operation became symptomatic after MPFL surgery may have been due to changes in compatibility and increased pressure in the PF joint after MPFL reconstruction. This is because a previous study reported that MPFL reconstruction reduced lateral patella tilt and another study reported that MPFL reconstruction increased the intra-articular pressure of the PF joint [6, 7]. Moreover, the synovial plica can become symptomatic as a result of surgery or trauma, and the surgical intervention in this case may have affected the onset of symptoms [5, 8].
Physical therapy is the initial treatment of medial synovial plica syndrome, and arthroscopic resection of plica is recommended if there is no improvement from physical therapy [5, 9]. In this present case, long-term postoperative physiotherapy was performed, but no improvement was observed. There are some reports on risk of intra-articular scarring and subsequent stiffness after plica resection, so we did not choose resection of the medial synovial plica at the arthroscopy in MPFL reconstruction [8]. However, it should be a viable option when the plica become symptomatic, and symptoms persist, because the arthroscopic resection of the synovial plica is minimally invasive and produces good mid-to-long term outcomes [9, 10].
We reported a case of plica syndrome following MPFL reconstruction that resulted in pain, which showed improvement after its removal. Surgeons should be aware of the possibility that asymptomatic synovial plica could become symptomatic after MPFL reconstruction. Furthermore, resection of the plica should be considered an option if it induces persistent pain.
Conflict of interest statement
None declared.



