-
PDF
- Split View
-
Views
-
Cite
Cite
Yurika Murase, Koji Kishimoto, Shoko Yoshida, Yuki Kunisada, Koichi Kadoya, Soichiro Ibaragi, Akira Sasaki, Surgical resection for advanced bisphosphonate-related osteonecrosis of the jaw associated with fibrous dysplasia: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa061, https://doi.org/10.1093/jscr/rjaa061
Close - Share Icon Share
Abstract
Bisphosphonate-related osteonecrosis of the jaw (BRONJ) is an adverse drug reaction represented by destruction and/or death of bone. Fibrous dysplasia (FD) is a rare bony disorder characterised by abnormal fibro-osseous tissue that has lowered resistance to infection. Effective treatments for BRONJ that follows FD are unclear. Here, we report that advanced BRONJ associated with FD was successfully treated by surgical resection. A 69-year-old woman, whose left maxillary bone showed a ground glass appearance on computed tomography (CT) images, was taking alendronate. At 1 year after teeth within the abnormal bone were extracted, exposed bone was observed in the extraction sites and CT images revealed separated sequestrums. Under the clinical diagnosis of Stage 2 BRONJ with FD, we performed not only sequestrectomy but also a partial resection of the FD. Thereafter, the healing was uneventful without recurrence. In conclusion, our case suggests that surgical resection is useful for advanced BRONJ associated with FD.
INTRODUCTION
Bisphosphonate-related osteonecrosis of the jaw (BRONJ) is a complication caused by bisphosphonate (BP) treatment for excessive bone resorptive diseases, such as osteoporosis and bone metastasis [1]. The histopathological findings of BRONJ were found to show necrotic bone and inflammation in the same manner as those of osteomyelitis of the jaw [2], whereas the pathophysiological mechanisms of BRONJ remain unclear [1]. Therefore, the management of BRONJ is difficult, which is a troublesome problem for oral and maxillofacial surgeons. Because standard treatments for BRONJ are not yet established, numerous studies have discussed the therapeutic strategies. Meanwhile, recent studies have suggested that surgical treatments are useful for Stages 2–3 BRONJ [1].
Fibrous dysplasia (FD) is a rare bony disorder affecting one bone or multiple bones, and the affected bones are generally conceived to be less resistant to infection [3]. Notably, FD of the jaw bone with dental infections may be complicated by osteomyelitis [3, 4].
There are no published reports describing surgical resection for BRONJ associated with FD, and the usefulness of surgical resection in such cases is unknown. Here, we demonstrate, for the first time, that Stage 2 BRONJ associated with FD was successfully treated by surgical resection.
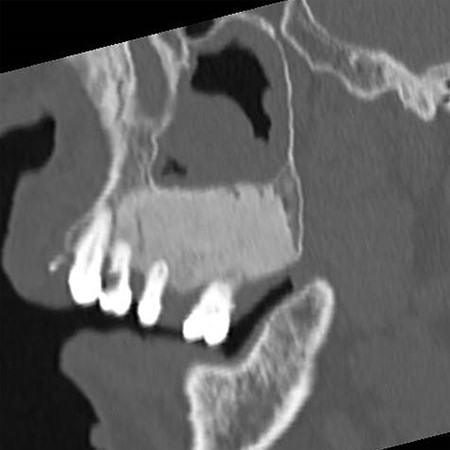
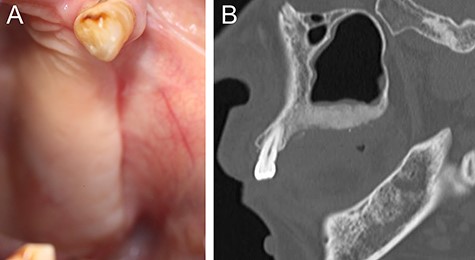
Sagittal section of CT image showing the maxillary bone with a ground glass appearance in distal regions from #24 part and bone resorption around #25 and #26.
CASE REPORT
A 69-year-old woman was referred to our hospital by a dentist at another hospital because of swelling in her left maxilla. There was the mobility of the left maxillary second premolar and first molar (FDI #25 and #26) and swelling of the surrounding gingiva. Computed tomography (CT) images revealed maxillary bone expansion with a ground glass appearance (Fig. 1). The patient had begun steroid therapy for polymyalgia rheumatica 4.5 years earlier. Since then she had been taking alendronate, one of the oral BPs, for the prevention of glucocorticoid-induced osteoporosis.
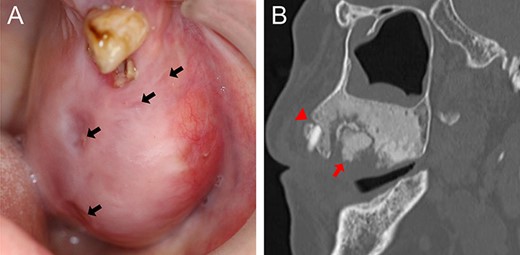
(A) Intraoral photograph showing gingival fistulas in #25 and #26 extraction sites (arrows). (B) Sagittal section of CT image showing separated sequestrums in the left maxilla (arrow) and bone resorption in the periapical area of #24 (arrowhead).
The clinical diagnosis was acute periodontitis in #25 and #26 parts with FD of the left maxillary bone. After an administration of clarithromycin, #25 and #26 were extracted, and then small bone fragments were collected from the sockets for a histopathological examination. The finding of not FD but the sequestrum predicted the occurrence of BRONJ.
At 1 year after the extractions, a purulent discharge and exposed bone with gingival fistulas were observed in the extraction sites (Fig. 2A). CT images revealed separated sequestrums in the left maxilla and bone resorption in the periapical area of the left maxillary first premolar (FDI #24) (Fig. 2B). With the permission of the patient’s attending physicians, the alendronate was withdrawn. After exposed bone had been observed for 8 weeks, the patient was clinically diagnosed with Stage 2 BRONJ accompanying FD of the left maxillary bone. Under general anesthesia, we first performed extraction of #24 and sequestrectomy. We then performed a partial resection of the FD because necrotic-like bone fragments were collected by curettage of the marginal bone (Fig. 3). Finally, the surgical wound was completely closed by sutures. The histopathological diagnosis was chronic osteomyelitis with FD (Fig. 4). At 2.5 years after the operation, the healing is uneventful although residual FD bone exists (Fig. 5). Although local conditions permit the resumption of alendronate, it remains discontinued at the attending physicians’ discretion.
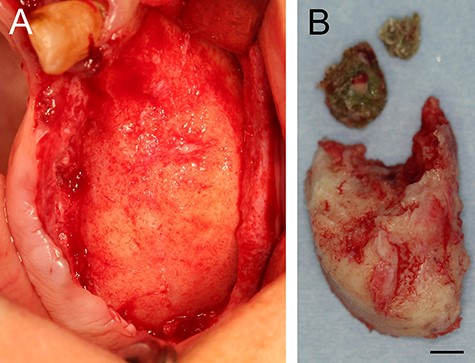
(A) Intraoral photograph showing a resected area. (B) Surgical specimens: separated sequestrums and resected FD bone (scale bar: 5 mm).
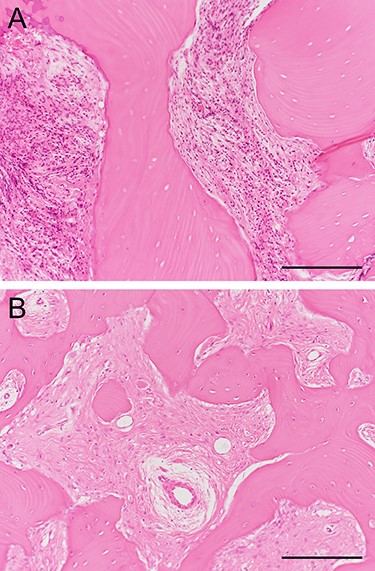
Photomicropraphs showing distinct histopathological findings in surgical specimens (hematoxylin-eosin stain, scale bar: 200 μm). (A) A marginal bone fragment of separated sequestrums showing necrotic bone with typical empty lacunae, surrounded by numerous inflammatory cells, and (B) resection margin showing irregularly shaped trabeculae of woven bone and proliferation of collagen fibers with fibroblasts but no necrotic bone and inflammatory cells.
(A) Six-month postoperative intraoral photograph showing complete healing of a surgical wound. (B) Sagittal section of CT image showing residual but not recurrently infected FD bone in the left maxilla after surgical resection.
DISCUSSION
In the current position paper, surgical treatments tend to be recommended for advanced BRONJ [1]. Surgical resection can produce higher cure rates than local debridement [5]. In our case, after local debridement including sequestrectomy, the residue of necrotic bone within marginal bone of the separated sequestrums was suspected; therefore, we added a partial resection of the FD. Indeed, the histopathological findings of marginal bone of the separated sequestrums shown in Fig. 4A proved the residues of necrotic bone and inflammation; in contrast, the histopathological findings of the resection margin shown in Fig. 4B found no necrotic bone and inflammation. As a result of adding the resection, the healing has been uneventful without recurrence although residual FD bone exists. Metwally et al. [6] reported the first cases of BRONJ associated with FD, in which only a Stage 2 case presented continual infection despite the combination of local debridement and antibiotic therapy. These findings suggest that surgical resection may be more useful than local debridement for advanced BRONJ associated with FD.
Our patient who had been taking an oral BP for years developed BRONJ after tooth extractions within FD bone. FD patients have been reported to develop BRONJ after tooth extractions within FD bone despite the long-term discontinuation of intravenous BPs [6]. These findings indicate that tooth extraction within FD bone may be a higher risk factor for BRONJ regardless of the presence/absence of the discontinuation of BPs.
The number of patients with FD complicated by BRONJ could increase, since FD patients can receive BP therapy for FD-related bone pain [6–8]. Our case supports aggressive treatment such as surgical resection for advanced BRONJ associated with FD. However, it remains unclear whether such a surgical treatment strategy is effective without the discontinuation of BP treatment. Further studies are needed in order to establish therapeutic strategies for BRONJ associated with FD.
Conflict of interest statement
None declared.
Financial support
None.



