-
PDF
- Split View
-
Views
-
Cite
Cite
Alexandra Stathis, John Gan, Traumatic arteriovenous fistula: a 25-year delay in presentation, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa042, https://doi.org/10.1093/jscr/rjaa042
Close - Share Icon Share
Abstract
A 64-year-old lady presented with a 6-month history of worsening unilateral leg swelling, with an audible bruit of the popliteal artery. Arterial duplex ultrasound confirmed the presence of an arteriovenous fistula (AVF) between the posterior tibial artery and vein. Upon thorough history, it was discovered that the patient had sustained a stab wound to this region some 25 years prior. The fistula was successfully managed endovascularly by means of a covered stent. This case highlights an unusual delayed presentation of an AVF and demonstrates the effectiveness of endovascular treatment of this condition.
INTRODUCTION
Arteriovenous fistulas (AVFs) are abnormal connections between arteries and veins, which divert blood flow to the low-pressure venous system. The most common cause of AVFs is iatrogenic injury by means of arterial access in the groin for endovascular procedures. While many fistulas will spontaneously resolve, large fistulas can result in clinically significant blood diversion requiring surgical intervention. Most fistulas will either resolve or become clinically significant within days to months after formation.
CASE REPORT
A 64-year-old lady was referred to our vascular service with a 6-month history of worsening left lower leg swelling and foot paraesthesia. There was no history of claudication, rest pain or ulceration. General examination demonstrated evidence of haemosiderin deposition of the lower leg and a small linear scar overlying the calf. History revealed the scar to be the result of a stab wound inflicted some 25 years prior. Further medical history included type 2 diabetes mellitus, hypertension, smoking, hepatitis C and previous IV drug use.
Physical examination confirmed that all pulses of the lower limb were palpable. On auscultation, a loud popliteal artery bruit was discovered.
Arterial duplex ultrasound identified an AVF between the posterior tibial artery and posterior tibial vein. It is likely that this patient developed a traumatic AVF secondary to the stab wound inflicted 25 years prior, and recent enlargement of the fistula had led to the development of symptoms.
Formal angiogram was undertaken and posterior tibial AVF was confirmed (Fig. 1). Two Advanta V12 polytetrafluoroethylene covered balloon-expandable stents were placed in the posterior tibial artery (Merrimack, NH, USA): 5 × 22 mm distally and 6 × 22 mm proximally, resulting in successful exclusion of the fistula (Fig. 2).
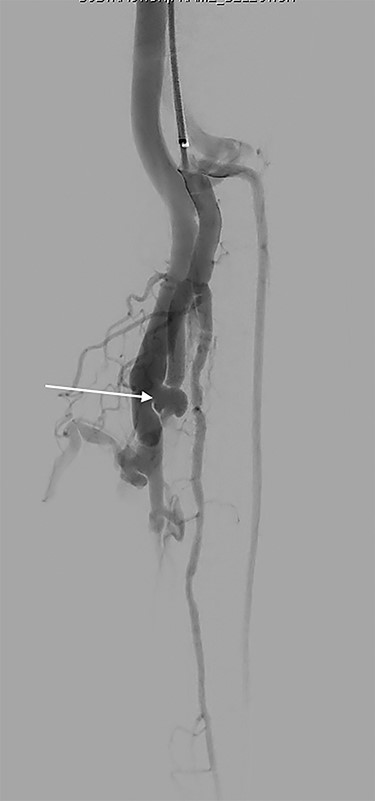
Focused angiography pre-intervention with a catheter positioned at the origin of the tibio-peroneal trunk (TPT). Contrast flows into the TPT, through the AVF (arrow) and into the venous system.
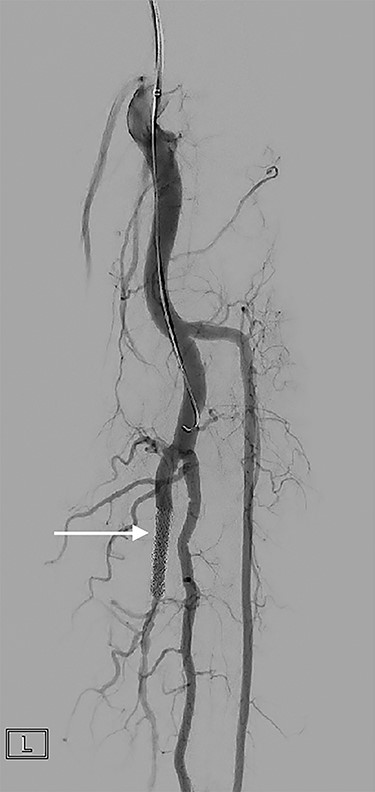
A covered stent (arrow) deployed in the posterior tibial artery occludes flow through the fistula. Contrast flows into the arterial tree without shunting into the venous system.
DISCUSSION
AVFs are abnormal connections between arteries and veins, which divert blood flow to the low-pressure venous system. Fistulas may be congenital or acquired and can occur almost anywhere within the body.
The most common cause of AVFs is iatrogenic injury by means of arterial access in the groin for endovascular procedures, where the incidence of traumatic AVF formation is estimated to be as high as 0.88% [1, 2]. Incidence is highest in therapeutic procedures compared with diagnostic, which likely reflects the calibre of the access sheath required [4]. Certainly, many of these are minute, clinically silent and resolve without ever being observed. A number of factors increase the risk of AVF formation, including increased BMI, advanced age, female gender and hypertension [3]. The use of ultrasound-guided puncture enables the direct visualisation of the target vessel and reduces the risk of inadvertent venous puncture.
Other causes of AVF formation include traumatic injuries such as blunt force, gunshot or stab wounds [1, 2].
Newly formed AVFs are usually asymptomatic and may remain as such for days to months, while the fistulous tract matures to a haemodynamically significant size. Symptoms arise from an increase in venous pressure or decreased distal arterial supply. These may include new or worsening varicose veins, oedema, claudication and formation of deep vein thrombosis [4, 5].
Clinical suspicion of an AVF may be high in the patient who presents with a pulsatile mass, palpable bruit or unilateral lower extremity oedema. Gold standard diagnosis is by means of duplex ultrasound, which demonstrates continuous flow and elevated diastolic velocities in the presence of an AVF, though CT angiography may also be useful [6]. Formal angiography can provide selective catheterisation and imaging of the affected vessels, as well as enabling therapeutic intervention.
While many asymptomatic AVFs will spontaneously resolve, intervention is indicated for clinically significant fistulas [1]. Surgical repair may be open or percutaneous and is based on the principle that the fistulous tract must be disconnected, obstructed or occluded. Open repair involves obtaining proximal and distal control of the fistula, division of the connection between artery and vein, followed by closure of both vessel defects [7]. The open approach is not without difficulty; the presence of dense scar tissue and venous hypertension can present a challenge for dissection and haemostasis.
Percutaneous approach involves the use of endovascular coils or glue to embolise the fistula—which requires a long fistulous tract in order to be feasible—or to deploy covered stent grafts that physically exclude the fistula from circulation [8]. Some AVFs may be amenable to ultrasound-guided compression whereby an ultrasound probe is utilised to apply sufficient force to occlude fistula flow without compromising distal perfusion [9].
Non-iatrogenic post-traumatic AVF formation is uncommon but should be considered in the patient with unilateral lower limb oedema, new varicosities or palpable bruit and a history of trauma. Endovascular management by means of covered stenting, as undertaken in this case, has been shown to be a safe and effective method for the management of traumatic AVFs.
Disclosure
This paper is the original work of the named authors and has not been previously presented or submitted for publication.
Conflict of interest statement
None declared.
References
Author notes
The corresponding author is an unaccredited surgical registrar and is not the recipient of a research scholarship.



