-
PDF
- Split View
-
Views
-
Cite
Cite
Joel Noutakdie Tochie, Landry Wakheu Tcheunkam, Collince Tchakounté, Nkengafac Nyiawung Fobellah, Samuel Nambile Cumber, First-trimester rupture of a gravid bicornuate uterus after prior vaginal deliveries, simulating a ruptured ectopic pregnancy: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa366, https://doi.org/10.1093/jscr/rjaa366
Close - Share Icon Share
Abstract
The first-trimester rupture of a bicornuate uterus (BU) is a rare obstetrical emergency, especially following previous normal vaginal deliveries where it is often misdiagnosed. A 24-year-old G3P2002 woman presented at 11 weeks of gestation with sudden onset of severe left iliac fossa pain without other symptoms. On examination, she was fully conscious and hemodynamically unstable with signs of peritoneal irritation, a distended pouch of Douglas and a slightly enlarged uterus and a tender left adnexal mass. The diagnosis of a ruptured ectopic pregnancy was made and a laparotomy was done. Intra-operative findings were hemoperitoneum, a left ruptured BU and a dead fetus. Surgical management entailed hysterorrarphy, left salpingectomy and conservation of both ovaries. Her postoperative course was uneventful and future fertility was preserved. We recommend a high index of suspicion of ruptured BU as a differential diagnosis of acute abdomen in the first trimester in women with previous term vaginal deliveries.
INTRODUCTION
Bicornuate uterus (BU) is a rare congenital uterine anomaly occurring at a prevalence rate of 0.4% in the general population [1]. In non-pregnant women, congenital uterine malformations like BU are associated with an increased fold of infertility, endometriosis, painful hematometra and urinary tract anomalies [1]. On the other hand, during gestation, BU may increase the risk of spontaneous abortions, preterm deliveries, cervical insufficiency and uterine rupture [1]. Rupture of a gravid BU is a rare obstetric emergency and it is the most dreaded complication of BU due to massive life-threatening hemorrhage which may be fatal to both the pregnant mother and fetus [2]. Furthermore, BU rupture during early gestation is quite rare and generally occurs during the second and third trimester of pregnancy [2]. Its most recommended treatment is surgical resection of the rudimentary ruptured horn or total hysterectomy if the latter is difficult to perform [2]. The case we present is among the few or perhaps the first reporting a first-trimester rupture of the rudimentary horn of a BU, occurring after two successive term normal vaginal deliveries, misdiagnosed for a ruptured ectopic pregnancy and managed by conservative surgery with an uneventful postoperative course and preserved fertility.
CASE REPORT
A 24-year-old African female at 11 weeks of pregnancy presented to our maternity unit with severe burning continuous left iliac fossa pain of sudden onset associated with vaginal spotting, two episodes of vomiting and no other symptom. Her past history was relevant for no chronic cyclic pelvic pain or severe dysmenorrhea. She also had two uneventful term normal vaginal deliveries to a 2600 g newborn and 2700 g neonate 5 and 2 years ago, respectively.
On examination, she was pale, ill-looking, hemodynamically unstable and temperature 36.8°C. There was mild abdominal distention, left iliac fossa and supra-pubic tenderness and guarding. On speculum examination, there was a single closed cervix with mild bleeding from its external os. Digital vaginal examination showed mild cervical motion tenderness, all fornices were fulled, the uterus was slightly enlarged and there was a tender left adnexal mass. An urgent 2D pelvic ultrasound scan revealed a slightly enlarged uterus (12 x 9 x 8 cm), with an emptied uterine cavity and a thick endometrium. Adjacent to the uterus, a gestational sac of ~7 x 6 cm containing a fetus corresponding to 11 weeks of pregnancy (Fig. 1). The fetus had no cardiac activity. The scan also showed free fluid in the Morrison’s pouch, the pelvis and abdomen estimated at 1300 mL. The diagnosis of a ruptured ectopic pregnancy was made. A pre-operative workup result is illustrated in Table 1.
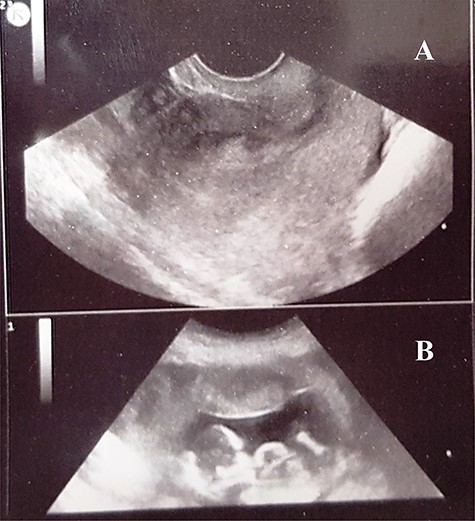
A 2D pelvic ultrasound scan showing a normal size uterus, with thick endometrium (A), peritoneal fluid, and an abdominally aborted gestational sac containing a dead embryo (B) mimicking a ruptured ectopic pregnancy.
| Laboratory test . | Values . | Reference values . | |
|---|---|---|---|
| . | on admission . | Day 1 postoperation . | . |
| White blood cell count (WBC) | 12 900 | 9800 | 4000–10 000/mm3 |
| Hemoglobin | 6.9 | 10.8 | 12–15 g/dl |
| Hematocrit | 20.6 | 32.4 | 35–49% |
| Platelet count | 286 000 | 202 000 | 150–400 000/mm3 |
| Prothromine time (PT) | 99 | – | 70–100% |
| Cephalokaoline time (TCA) | 32 | – | 28–33 s |
| Serum urea | 0.39 | 0.39 | 0.35–0.45 g/l |
| Serum creatinine | 8.9 | 9.2 | 6–13 mg/l |
| Blood group | B rhesus positive | – | – |
| Laboratory test . | Values . | Reference values . | |
|---|---|---|---|
| . | on admission . | Day 1 postoperation . | . |
| White blood cell count (WBC) | 12 900 | 9800 | 4000–10 000/mm3 |
| Hemoglobin | 6.9 | 10.8 | 12–15 g/dl |
| Hematocrit | 20.6 | 32.4 | 35–49% |
| Platelet count | 286 000 | 202 000 | 150–400 000/mm3 |
| Prothromine time (PT) | 99 | – | 70–100% |
| Cephalokaoline time (TCA) | 32 | – | 28–33 s |
| Serum urea | 0.39 | 0.39 | 0.35–0.45 g/l |
| Serum creatinine | 8.9 | 9.2 | 6–13 mg/l |
| Blood group | B rhesus positive | – | – |
| Laboratory test . | Values . | Reference values . | |
|---|---|---|---|
| . | on admission . | Day 1 postoperation . | . |
| White blood cell count (WBC) | 12 900 | 9800 | 4000–10 000/mm3 |
| Hemoglobin | 6.9 | 10.8 | 12–15 g/dl |
| Hematocrit | 20.6 | 32.4 | 35–49% |
| Platelet count | 286 000 | 202 000 | 150–400 000/mm3 |
| Prothromine time (PT) | 99 | – | 70–100% |
| Cephalokaoline time (TCA) | 32 | – | 28–33 s |
| Serum urea | 0.39 | 0.39 | 0.35–0.45 g/l |
| Serum creatinine | 8.9 | 9.2 | 6–13 mg/l |
| Blood group | B rhesus positive | – | – |
| Laboratory test . | Values . | Reference values . | |
|---|---|---|---|
| . | on admission . | Day 1 postoperation . | . |
| White blood cell count (WBC) | 12 900 | 9800 | 4000–10 000/mm3 |
| Hemoglobin | 6.9 | 10.8 | 12–15 g/dl |
| Hematocrit | 20.6 | 32.4 | 35–49% |
| Platelet count | 286 000 | 202 000 | 150–400 000/mm3 |
| Prothromine time (PT) | 99 | – | 70–100% |
| Cephalokaoline time (TCA) | 32 | – | 28–33 s |
| Serum urea | 0.39 | 0.39 | 0.35–0.45 g/l |
| Serum creatinine | 8.9 | 9.2 | 6–13 mg/l |
| Blood group | B rhesus positive | – | – |
Initial management consisted of fluid resuscitation, blood transfusion and intravenous (IV) analgesics. This was followed by an emergency laparotomy whose intra-operative findings were; hemoperitoneum of 2000 mL, a bicornis unicollis uterus with a 7 × 4 cm corporal rupture of a left ruptured rudimentary horn, a dead fetus and a right functional horn (Fig. 2). The uterine cervix was communicating with both uterine horns. Intra-operative management consisted of draining the hemoperitoneum, delivery of the dead fetus and its placenta, hysterorrarphy (Fig. 3), left salpingectomy, conservation of both ovaries and abdominal wall closure.
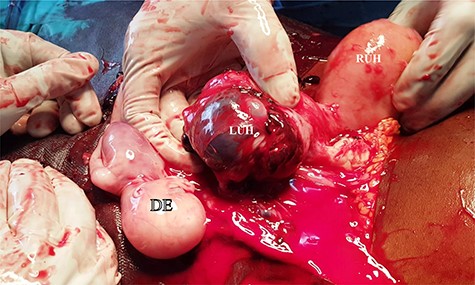
Intra-operative findings; hemoperitoneum, a bicornate uterus with a left non-communicating ruptured corporeal atrophic rudimentay uterine horn (LUH), a dead embryo (DE), an intact right uterine horn of normal size.

Hysterorraphy at the level of left uterine horn corpus. Frontal view (A), and lateral view (B).
Her postoperative recovery was uneventful. The patient was discharged on the fifth postoperative day. She was counseled to use oral conceptive pills for at least 1 year. Oral contraceptives were stopped 14 months postoperation when she had a desire of pregnancy. Following close antenatal follow-up, she delivered a female neonate weighing 2870 g at 37 weeks of gestation from the right communicating uterine horn 2 years later.
DISCUSSION
The peculiarities of this case lie in it’s first-trimester presentation, its occurrence after two prior successive term normal vaginal deliveries and its atypical, yet successful management as evident by a regular postoperative recovery and preserved fertility.
Overall, clinical features which should help suspect a ruptured gravid BU are first-trimester pregnancies, a multigravida pregnant women with a past history uterine surgeries (e.g. cesarean section, myomectomy), onset of severe continuous pelvic pains presenting as an acute abdomen with signs of peritoneal irritation, signs of anemia and shock due to hemoperitoneum [1, 3]. We had a low index of clinical suspicion of a ruptured gravid horn of a BU owing to the scarcity of epidemiology data on this pathology in Africa; its clinical presentation which mimicked a ruptured ectopic pregnancy and misdiagnosis of a ruptured ectopic gestation on 2D pelvic sonography. This re-iterates the common diagnostic challenges of congenital uterine malformations and obstetrical emergencies encountered in low-resource settings [4–6].
The treatment of a ruptured gravid rudimentary horn of a BU advocated by most authors entails surgical resection of the ruptured horn preferably via laparoscopic surgery [2, 3] to prevent the risk of recurrent rupture in case of future pregnancy within the same rudimentary horn [7]. Considering the large amount of hemoperitoneum, open surgery appeared to be the preferred surgical approach in our patient. Most gravid rudimentary horn ruptures occur between first and second trimester as a result of insidious myometrial thinning with advancing gestational age [8]. Hence, resection of the gravid rudimentary horn, ipsilateral salpingectomy and conserving the ovary are the recommended surgical management for women desiring to maintain their fertility potential [8]. With an extensive literature search, to the best of our knowledge, this case is the first report describing a conservative surgical approach (hysterorrarphy, left salpingectomy and conservation of both ovaries) for ruptured BU, which seemed effective as evident by the uneventful postoperative course, a preserved postoperative fertility and reduced risk of BU rupture recurrence in the subsequent gestation [9].
To end, this case shows that uterine rupture can occur as early as 11 weeks when associated with a uterine malformation like BU; conservative surgery is feasible and is associated with preserved fertility if contraceptives are taken for at least a year. As seen, its clinical presentation mimics ruptured ectopic pregnancy, hence, can easily be misdiagnosed and a high index of the clinical suspicion cannot be overemphasized.
CONFLICT OF INTEREST OF STATEMENT
None declared.
FUNDING
None.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images.



