-
PDF
- Split View
-
Views
-
Cite
Cite
Miguel Johnson, Lorna Cook, Fabio Rapisarda, Riccardo Bonomi, Dibendu Betal, Surgical dilemma of the management of breast cancer in a patient with neurofibromatosis: case report and a review of the literature, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa365, https://doi.org/10.1093/jscr/rjaa365
Close - Share Icon Share
Abstract
Neurofibromatosis type 1 (NF-1)—also commonly known as Von Recklinghausen’s disease—is an autosomal dominant disease that represents a constellation of clinical features. There are well-established links between NF-1 and many tumors; however, the link between NF-1 and breast cancer has more recently been elucidated. While the management of breast cancer is generally well established, there are unique challenges noted in patients with NF-1. There may be delayed presentations due to difficulty in differentiating underlying neurofibroma from a sinister breast mass. Additionally, multiple skin lesions seen in NF-1 create challenges in the interpretation of mammography. Furthermore, a surgical conundrum is created, as these patients appear to have a higher risk of angiosarcoma following radiotherapy. A mastectomy may be the best option as it obviates the need for radiation therapy and ongoing surveillance. A case exemplifying these dilemmas and a review of the literature are presented.
INTRODUCTION
Neurofibromatosis type 1 (NF-1)—also commonly known as Von Recklinghausen’s disease—represents a constellation of clinical features based on the National Institute of Health diagnostic criteria [1]. NF-1 is an autosomal dominant condition and is usually due to a genetic defect in the NF1 gene [2].
Surgical intervention is usually required in many well-established conditions associated with NF-1 including malignancies such as malignant peripheral nerve sheath tumors, pilocytic astrocytomas of the optic radiation, gastrointestinal stromal tumors (GISTs), rhabdomyosarcoma and pheochromocytoma [3]. More recently, the link between NF-1 and breast cancer has become well established, with findings suggestive of a higher risk of contralateral breast cancer and an overall poor survival [4, 5].
Typically, surgical management of breast cancer may involve mastectomy or breast conservative surgery (BCS) involving wide local excision—introduction of oncoplastic techniques has allowed larger tumors to be safely resected with satisfactory aesthetic outcomes. Systemic treatment may include radiotherapy, chemotherapy, monoclonal antibody and endocrine therapy.
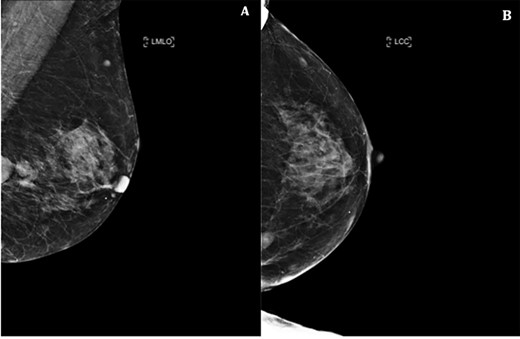
Left mammogram showing masses—A. Mediolateral oblique B. Cranial–caudal views.
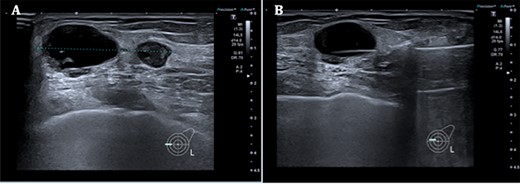
A. Left breast ultrasound showing two lesions at the 9 o’clock position measuring a total distance of 37 mm. B. Core biopsy done of the main lesion.
The management of breast cancer in patients with NF-1 is less clear and presents unique challenges due to the diagnostic challenges as well as the aggressive nature of breast cancer in these patients. Additionally, there is a theoretical risk of radiation-induced sarcomatous changes if radiotherapy is administered after breast conservative surgery [6]. This creates a surgical dilemma in this unique group of patients. We present a case of a patient known to have NF-1 who subsequently developed breast cancer, and a brief review of the literature.
CASE PRESENTATION
A 69-year-old woman known to have a diagnosis of neurofibromatosis presented with 1 week history of left breast lump increasing in size, with no new skin or nipple changes. She was post-menopausal with no previous HRT use, no previous breast problems and no family history of breast or ovarian cancers but has a strong family history of neurofibromas. She was asthmatic but otherwise fit and well. Her previous screening mammogram done in 2017 showed no suspicious features.
Triple assessment was done—examination revealed multiple cutaneous neurofibromas in keeping her NF1. Breast examination revealed a firm irregular 2-cm lump at the 9 o’clock position of the left breast with no contralateral lumps nor any evidence of lymphadenopathy. Bilateral mammogram demonstrated a dense indeterminate mass on the left breast (Fig. 1). Targeted ultrasound scan showed two cystic-like lesions adjacent to each other (Fig. 2). A core needle biopsy was done of the larger lesion confirming grade 3 invasive ductal carcinoma—receptor status analysis revealed that the lesion was ER negative, PR negative and HER2 positive.
Following a multidisciplinary team meeting (MDT), the clinical decision was to proceed with a left mastectomy and sentinel lymph node biopsy (Fig. 3). The surgical procedure was uneventful, and the patient had a normal healing process with a favorable evolution. Histopathological assessment confirmed multifocal Grade 3 invasive ductal carcinoma in the same quadrant (17 and 10 mm) with lymphovascular invasion. Sentinel lymph node analysis revealed no metastatic involvement of the seven lymph nodes excised. Following surgical resection, MDT re-discussion recommendation was for adjuvant chemotherapy, trastuzumab and bisphosphonates. Surgical follow-up will be 5 years of clinical follow-up and mammogram on the contralateral breast.
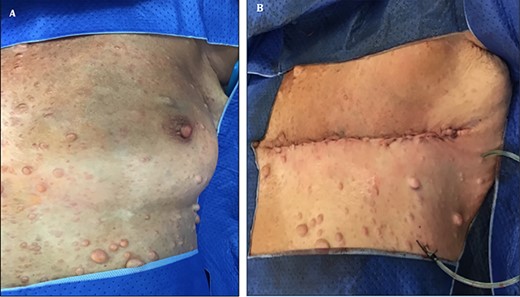
Photograph showing multiple neurofibroma in patient with NF-1 A. Pre- and B. Post-left mastectomy and sentinel lymph node biopsy.
DISCUSSION
The diagnosis of NF-1 is usually based on clinical findings [1]. Heterozygous pathogenic variants in NF1 are responsible for neurofibromatosis 1 [7]. Molecular genetic testing of NF1 is rarely needed for diagnosis. While surgical intervention in the NF-1 patient is well established for some associated conditions, the link between breast cancer and NF-1 has more recently been confirmed [4, 5].
Patients with NF-1 gene mutations appear to confer a higher overall lifetime risk of any cancer in comparison to the general population. Furthermore, both the overall mortality and breast cancer-specific mortality appears to be higher among women with NF1 in a Finnish population study. These patients also appear to have a more aggressive presentation with 4–11-fold higher risk of contralateral breast cancer [5].
The management of breast cancer in these patients presents some dilemmas that are unique to this cohort. There may be a delay in presentation due to difficulty in differentiating underlying neurofibromas and a sinister breast mass. Similarly, the presence of multiple cutaneous neurofibromas with coexisting breast cancer may make interpretation of mammography particularly challenging [8].
A review of the literature demonstrates several articles highlighting the relationship between breast cancer and neurofibromatosis, however; to the best of the authors’ knowledge, similar paper discussing the surgical dilemma in management of these patients appears to be limited. Hasson et al. presented a case where breast conservative treatment was initially considered but was later thwarted and a mastectomy was performed [9]. Similarly, Salemis and Nakos reported a case of a delayed presentation of breast cancer in a patient with NF-1 as patient thought her mass was a manifestation of her known NF-1 disease. They later performed a mastectomy as their surgical choice [10].
While breast conservative surgery appears to be a safe alternative to mastectomy generally. It confers, at least theoretically, unique risk of the development of radiation-induced sarcomatous changes in patients with NF-1. Moreover, patients with NF-1 tend to have more aggressive breast cancers, as evidenced by higher tumor grades and the higher incidence of contralateral disease. Additionally, given the diagnostic challenges of evaluation of the breast during screening and surveillance, a mastectomy may serve as the best choice in these patients as obviates the need for radiation therapy to the breast and the potential sarcomatous sequelae.
In view of the paucity of data in unique cohort of patients, randomized controlled trials are needed to further elucidate the best management strategies and the safety of breast conservative surgery.
CONCLUSION
Neurofibromatosis presents not only diagnostic challenges but also a unique surgical dilemma for the patient and surgeon. While breast conservative therapy is an option in the management of breast cancer patients, systemic radiotherapy may theoretically lead to radiation induced secondary cancers in-patient with NF-1. In addition there are challenges to clinical surveillance of possible cutaneous recurrences and surveillance imaging.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



