-
PDF
- Split View
-
Views
-
Cite
Cite
Ibtisam Hasan, Stephanie F Smith, Amy Hammond-Kenny, Potts puffy tumour: a rare but important diagnosis, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz099, https://doi.org/10.1093/jscr/rjz099
Close - Share Icon Share
Abstract
Potts puffy tumour (PPT) is a subperiosteal abscess arising from frontal bone osteomyelitis. We present a case of a 75-year-old lady with headache and a forehead swelling who was initially treated for sinusitis and giant cell arteritis in a primary care setting, but failed to improve. Following clinical deterioration and further investigation, CT appearances were consistent with a diagnosis of PPT and an extra-axial collection. Needle decompression, frontal trephine and endoscopic frontal sinusotomy were performed and intraoperative swabs cultured Streptococcus constellatus PPT is an unusual clinical entity that benefits from prompt antibiotic and surgical management, and therefore early recognition is paramount. We highlight that PPT should be a differential diagnosis in all patients presenting with forehead or frontal swelling. Use of radiological imaging (CT/MRI) is necessary to not only confirm a diagnosis of PPT but to identify further intracranial complications, which can be life-threatening.
INTRODUCTION
Potts puffy tumour (PPT) is a pseudo-inflammatory tumour characterized by a forehead swelling resulting from subperiosteal abscess associated with frontal bone osteomyelitis. It was first identified by Sir Percival Potts in 1768, after whom it was eponymously named, when it was initially recognized as a complication of trauma directly to the forehead [1]. It is most commonly associated with chronic frontal sinusitis and head trauma [2]. Cases of PPT have been seen in all ages however it predominantly occurs in the adolescent age group, which is believed to be due to the peak of vascularity in the diplopic circulation during adolescence [3]. PPT has become exceedingly rare following the advent of broad-spectrum antibiotics, however, as it is a particularly unusual clinical entity that benefits from prompt surgical and antibiotic management, rapid recognition is imperative.
CASE REPORT
A 75-year-old female consulted her general practitioner with a 1 month history of right-sided fronto-temporal headache associated with nausea. On physical examination, she had a small, fluctuant swelling on the right side of her forehead. Past medical history was noteworthy for a right partial temporal craniectomy and evacuation of a traumatic haematoma following a head injury 5 years prior to presentation. Blood samples were taken on this encounter which revealed an elevated erythrocyte sedimentation rate of 52 mm and raised C-reactive protein of 24 mg/L. Full blood count and clotting screen were within normal limits. She was started on a short course of high dose prednisolone for presumed giant cell arteritis, which provided temporary symptomatic relief.
A fortnight later she represented with green nasal discharge, worsening frontal headache and an increase in the size of forehead swelling to 4 × 3 cm2. She was treated for presumed sinusitis with a week of oral doxycycline, followed by a 2-week course of co-amoxiclav for a presumed infected sebaceous cyst. Whilst awaiting an outpatient computerized tomography of the head, the swelling continued to increase in size and a deterioration in her memory occurred.
As demonstrated in Fig. 1, the computerized tomography imaging of the head revealed a right-sided subperiosteal forehead collection and a right-sided extra-axial collection with underlying frontal lobe oedema, associated with erosion of the anterior and posterior wall of the right-sided frontal sinus.
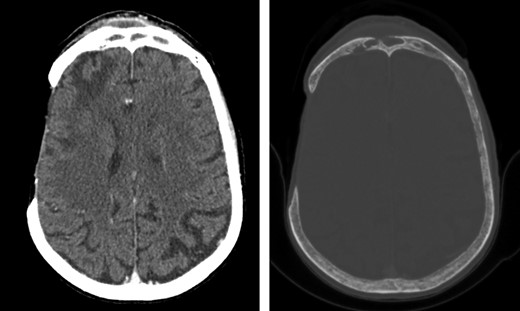
Axial computed tomography images of the head (left: brain window; right: bone window) showing a right-sided subperiosteal forehead collection and a right-sided extra-axial collection with underlying frontal lobe oedema, associated with erosion of the anterior and posterior wall of the right-sided frontal sinus. The images also show the previous right-sided temporal craniectomy defect with gliotic changes.
The patient was urgently referred to hospital. On admission, serology showed an elevated leucocyte count of 12.4 × 109/L (Neutrophils raised to 10.9 × 109/L) and a raised C-reactive protein of 84 mg/L. She was reviewed by the ENT team who performed needle aspiration in the emergency department. A 10 mL of foul-smelling purulent fluid was aspirated from the forehead swelling, which was sent for microscopy, sensitivity and culture. After seeking a Microbiology opinion, empirical ceftriaxone treatment was initiated. This was followed by a bedside incision and drainage of a further 17 mL of purulent fluid. Culture subsequently reveald growth of Group A Streptococcus.
Incision and drainage was repeated 3 days later and a corrugated drain was inserted. She was transferred to a tertiary centre for further management. Bilateral frontal sinus trephination and endoscopic frontal sinusotomy were performed. A swab was obtained and sent for microbiology, and a saline washout was performed of both sinuses. The corrugated drain was removed. Culture of the swab revealed a heavy growth of Streptococcus constellatus. Post-operative recovery was uncomplicated. A peripherally inserted central catheter (PICC line) was inserted and the patient was discharged with outpatient parenteral antibiotic therapy, which consisted of a further 6-week course of ceftriaxone.
DISCUSSION
PPT is serious complication of frontal sinusitis. Remained untreated, vascular compromise and secondary thrombophlebitis may occur causing bony necrosis with risk of intracranial extension including meningitis, subdural empyema, epidural abscess, subarachnoid inflammation or involvement of the brain parenchyma [4].
The most common presentations of PPT involve forehead swelling, headaches and nasal congestion and discharge [5]. Symptoms indicative of raised intracranial pressure such as lethargy, obtundation, nausea and vomiting have been reported as well as seizures [6]. These are concerning as they are suggestive of intracranial extension.
Contrast-enhanced CT is usually the initial imaging of choice for PPT [7] providing information on bony and intracranial involvement; magnetic resonance imaging can further demarcate the extent of this [8]. We note the time interval in this case between symptom onset and the decision to investigate with axial imaging, contributing to delayed diagnosis and treatment.
Culture of abscess fluid may reveal mixed polymicrobial growth with the most common causative bacterial pathogens including Streptococcus species, Staphyloccoccus aureus but also anaerobic organisms (such as Fusobacterium) especially in cases of intracranial involvement [9]. Cases with Haemophilius influenza, Enterococcus, Pseudomonas, Escherichiacoli and one case with Pasteurella multocida have also been reported [3]. Broad-spectrum antibiotic use is therefore recommended with a post-operative regime of long term antibiotic for a duration between 6 and 8 weeks. In this patient, swab culture had revealed S. constellatus, which was covered by the use of parenteral broad-spectrum antibiotics. To our knowledge, this species has been isolated from a PPT associated abscess in only one previous case [10].
In conclusion, it is imperative consider the complications of frontal sinusitis in patients who present with forehead swelling, headache and symptoms of raised intracranial pressure. Timely diagnosis and management of PPT permits better prognosis and avoids further complications.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- antibiotics
- magnetic resonance imaging
- edema
- giant cell arteritis
- endoscopy
- headache
- abscess
- differential diagnosis
- forehead
- intraoperative care
- primary health care
- sinusitis
- surgical procedures, operative
- diagnosis
- diagnostic imaging
- neoplasms
- pott's puffy tumor
- needle decompression for tension pneumothorax
- streptococcus constellatus
- clinical deterioration



