-
PDF
- Split View
-
Views
-
Cite
Cite
Konstantinos Tigkiropoulos, Ioannis Lazaridis, Kyriakos Stavridis, Marianthi Tympanidou, Dimitrios Karamanos, Nikolaos Saratzis, Inferior gluteal artery surgical access for embolization of large internal iliac artery aneurysm in a hostile abdomen, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz098, https://doi.org/10.1093/jscr/rjz098
Close - Share Icon Share
Abstract
Internal iliac artery aneurysms (IIAA) are a rare entity compared with all aortoiliac aneurysms. Continuous expansion due to retrograde flow from runoff vessels can lead to rupture with devastating results. Exclusion of the aneurysm represents a challenging procedure especially if the access is limited and the patient has a history of reoperations in the pelvic region.
A 78-year-old man with a history of endovascular aortic repair, coverage of internal iliac arteries and right hemicolectomy for adenocarcinoma of ascending colon presented with a rapidly expanding right IIAA (8.8 cm) due to type II endoleak. He successfully treated with coil embolization through inferior gluteal artery surgical access.
Inferior gluteal artery surgical access for embolization of internal iliac aneurysms in patients with hostile abdomen or in cases where antegrade route has already been excluded, is a feasible technique.
INTRODUCTION
Internal iliac artery aneurysms (IIAA) are a rare entity compared with all aortoiliac aneurysms. Its prevalence is estimated as 0.03% representing 0.3% of all aneurysms in the aortoiliac system [1]. Nowadays, endovascular aortic aneurysm repair (EVAR) has become the treatment of choice in high risk patients with aortoiliac aneurysms and appropriate anatomy. However, complications after EVAR especially type II endoleak, where flow into the aneurysm sac is maintained through retrograde flow from collateral vessels remains an important issue especially when there is a significant expansion of the sac increasing the risk of rupture. We present a case of successful embolization of 8.8 cm right IIA through inferior gluteal artery surgical access in a patient previously treated with EVAR for abdominal aortic aneurysm (AAA) and right hemicolectomy for adenocarcinoma of ascending colon.
CASE REPORT
A 78-year-old man was referred in our vascular unit due to an 8.8 cm right IIAA. His medical history included arterial hypertension, diabetes mellitus (non-insulin dependent), right hemicolectomy for adenocarcinoma of ascending colon and EVAR of abdominal aortic aneurysm with Anaconda stent graft (Anaconda, Vascutek, Scotland) 6 years ago followed by deployment of extensions in external iliac arteries with coverage of internal iliac arteries 1 year later in another facility. The patient did not refer any buttock claudication or intestinal disturbances during follow-up. The last control with computed tomography angiography was performed 4 years ago (CTA) depicting a right IIAA, 4.3 cm, which was decided to be managed conservative due to his medical comorbidities. A contrast-enhanced CT was performed in our unit which revealed an 8.8 cm right IIAA with the presence of two runoff vessels deep in the pelvis with direction to the gluteal muscles (Fig. 1). An endovascular embolization of the aneurysm was decided due to his medical history. The patient was fully informed for the endovascular repair, the possible complications of the operation and written consent was obtained.

Contrast-enhanced CT depicted an increase of right IIA to 8,8 cm with type II endoleak from two runoff vessels deep in the pelvic cavity.
OPERATION
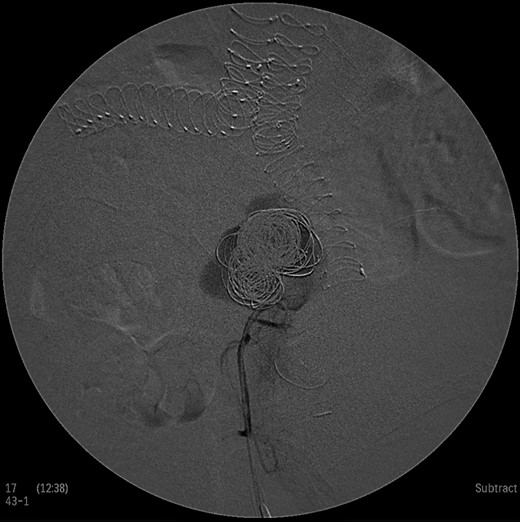
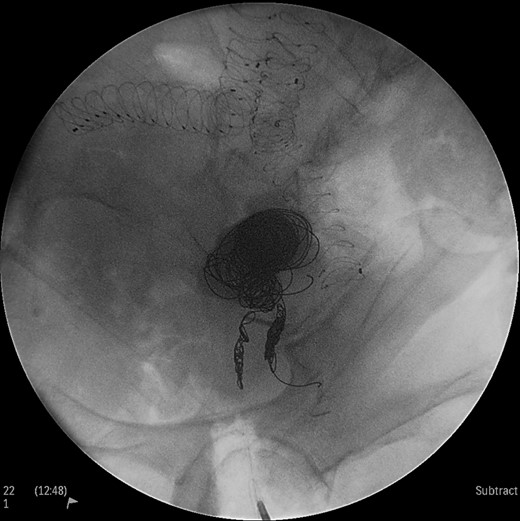
Under general anesthesia the patient was placed in prone position and a 15 cm transverse incision, slightly curvy was performed in the middle part of the right gluteal region between the posterior superior iliac spine and ischiac tuberosity. The gluteus maximus muscle was split and the inferior gluteal artery was identified as it entered the gluteal region through the greater schiatic foramen near the schiatic nerve below the piriformis muscle. The inferior gluteal artery was punctured using Seldinger technique and a 4Fr was introduced into the artery (Fig. 2). An angiography was made revealing the aneurysm of the right IIA and two feeding arteries, inferior gluteal artery and probably a branch of superior gluteal artery, filling the sac (Fig. 3). A 0.014 inch Pilot guide wire (Boston Scientific Corporation, USA) was inserted into the aneurysm and a microcatheter 3 Fr RENEGADE STC (Boston Scientific Corporation, USA) was advanced over the wire. After removing the wire, embolization microcoils (Interlock, Boston Scientific, USA) (two coils 22–600 mm, two coils 20–500 mm, three coils 18–500 mm) were introduced into the aneurysm sac (Fig. 4). A 5 Fr sheath was subsequently placed, a 5Fr RIM catheter (Cordis, USA) was advanced to the aneurysm sac through a 0.035 inch Terumo guide wire (Glidewire, Terumo Corporation, Japan) and selective catheterization of the second feeding artery was performed (Fig. 5). Embolization coils (Interlock, Boston Scientific, USA) were inserted into the two feeding arteries (two coils 15–400 mm) (Fig. 6). Completion angiogram depicted absence of blood flow into the aneurysm and the runoff vessels (Fig. 7). The patient had an uneventful recovery period without buttock claudication, ischemic complications and discharged in good condition. A follow-up CT aortography after 6 months depicted complete thrombosis of the aneurysm (Fig. 8).
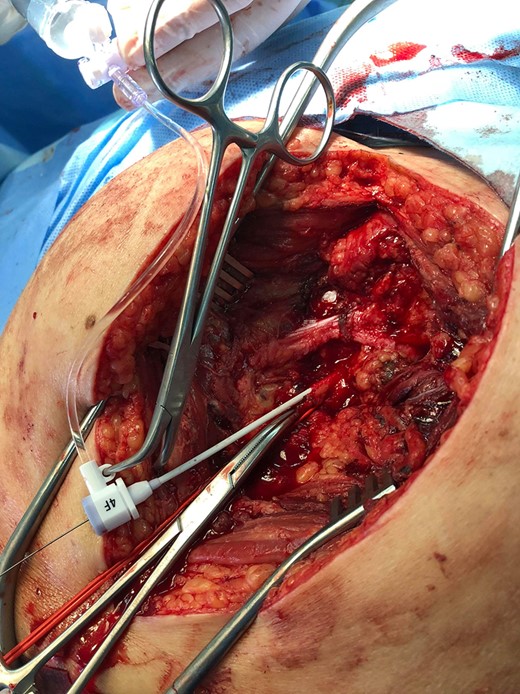
Posterior surgical access to the aneurysm, a sheath is inserted in the inferior gluteal artery.

Intraoperative angiogram showing the presence of the aneurysm and two collateral vessels, embolization with coils of the sac and two feeding arteries. Completion angiogram depicted absence of blood flow in the IIA aneurysm and the runoff arteries.

Intraoperative angiogram showing the presence of the aneurysm and two collateral vessels, embolization with coils of the sac and two feeding arteries. Completion angiogram depicted absence of blood flow in the IIA aneurysm and the runoff arteries.
Intraoperative angiogram showing the presence of the aneurysm and two collateral vessels, embolization with coils of the sac and two feeding arteries. Completion angiogram depicted absence of blood flow in the IIA aneurysm and the runoff arteries.
Intraoperative angiogram showing the presence of the aneurysm and two collateral vessels, embolization with coils of the sac and two feeding arteries. Completion angiogram depicted absence of blood flow in the IIA aneurysm and the runoff arteries.
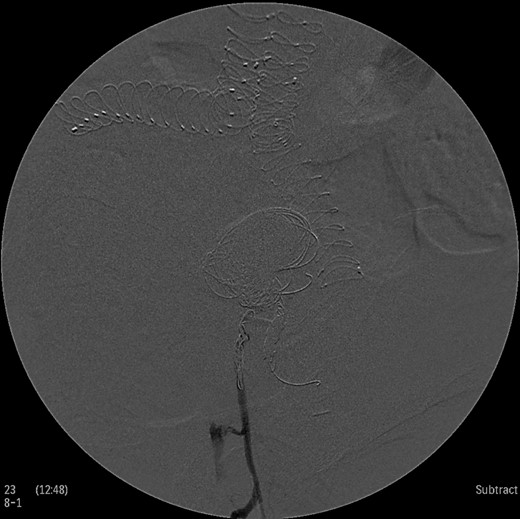
Intraoperative angiogram showing the presence of the aneurysm and two collateral vessels, embolization with coils of the sac and two feeding arteries. Completion angiogram depicted absence of blood flow in the IIA aneurysm and the runoff arteries.
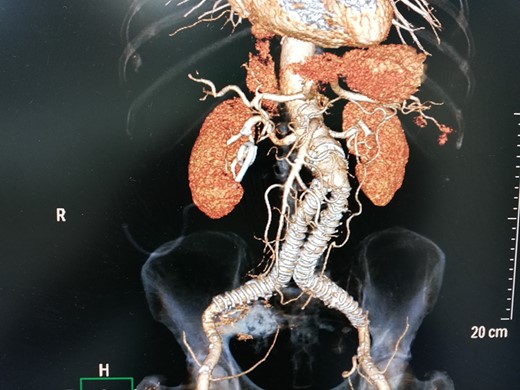
3D-CT aortography after 6 months depicted thrombosis of the aneurysm with coil embolization.
DISCUSSION
Endovascular repair of IIA aneurysms includes stent graft placement, coil embolization or combination of both [2, 3]. The lower periprocedural morbidity and mortality makes it the treatment of choice in high risk patients with serious comorbidities with acceptable rates of short and midterm of patency compared to open surgery [4]. However, there are a number of situations, endograft iliac extensions to the external iliac arteries or laparotomies for abdominal surgical pathologies where antegrade access to the IIA is not possible and posterior approach to the aneurysm through collateral arteries provides a significant alternative route for endovascular treatment of IIA aneurysms. The method was firstly described in 1985 and since then a variety of techniques (ultrasound-guided, CT-guided, open retroperitoneal) have been described for access and embolization of the sac [5–8].
Surgical access to the inferior gluteal artery necessitates a thorough evaluation and comprehension of the pelvic anatomy. After surgical cutdown of the buttock and splitting of the gluteus maximus muscle, piriformis muscle is identified which constitutes an important anatomic landmark separating inferior and superior gluteal arteries which enter the gluteal region through greater schiatic foramen. Catheterization of the IIA sac can then be gained through gluteal arteries in retrograde manner. Our patient had a history of EVAR 6 years ago followed by stent graft extension to the external iliac arteries 1 year later in another facility. There is still a question why the hypogastric aneurysms were not embolized during EVAR. Despite proximal exclusion of IIA, type II endoleak through runoff vessels permitted expansion of the right IIA aneurysm increasing the risk of rupture. Embolization through posterior approach and surgical access of inferior gluteal artery was used effectively in a patient with a hostile abdomen. The patient did not experience any buttock claudication or ischemic complications postoperatively after embolization and follow-up CTA revealed thrombosis of right hypogastric aneurysm.
CONCLUSION
Inferior gluteal artery surgical access for embolization of internal iliac aneurysms, especially in patients with hostile abdomen or in cases where antegrade route for catheterization of the sac has already been excluded from previous endovascular procedures is a feasible technique with promising results. However more studies are necessary to establish its efficacy.
CONFLICT OF INTERESTS
None.
FUNDING
The funding agency provides technical support in our vascular unit during endovascular procedures.
CONSENT
Written informed consent was obtained from the patient for publication of this case report.



