-
PDF
- Split View
-
Views
-
Cite
Cite
Han Nien Beh, Yuni Fitri Ongso, Simultaneous gastric and colonic erosions from gastric band and its tubing in the setting of recurrent intra-abdominal infection, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz102, https://doi.org/10.1093/jscr/rjz102
Close - Share Icon Share
Abstract
Chronic abdominal pain is often a diagnostic dilemma. We present a 59-year-old female with chronic generalized colicky abdominal and altered bowel habits. She was investigated with colonoscopy and CT abdomen. Patient has a history of recurrent diverticulitis and insertion laparoscopic adjustable gastric band. The colonoscopy revealed a tubular foreign body and diverticular disease. The tubular structure was confirmed to be gastric band tubing on CT abdomen, also showing simultaneous gastric and colonic erosions. She denies any gastric band port related infection or previous issues with gastric band. This case suggest that the cause of the erosion is due to recurrent episodes diverticulitis. She underwent wedge resection of large bowel and laparoscopic removal of gastric band. She had uneventful post-operative recovery.
INTRODUCTION
Abdominal pain of unknown cause is often a diagnostic dilemma. Patients with background of bariatric surgery should be investigated promptly for procedure related complications. Patients can present acutely in the Emergency department with acute abdomen or in the outpatient setting where patients have chronic abdominal pain. In this particular case, we have found the cause of the patient’s chronic abdominal pain contributed by erosion of gastric band tubing likely related to diverticulitis.
CASE REPORT
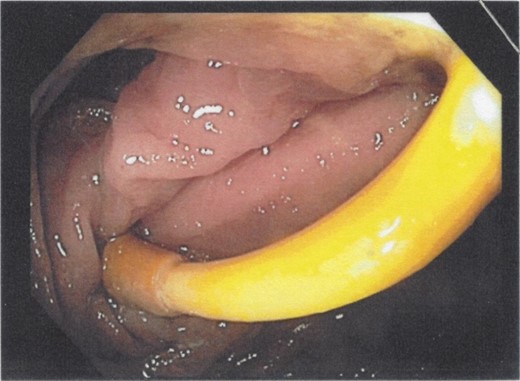
A 59-year-old female patient presented to her local family doctor with chronic generalized intermittent colicky abdominal pain and altered bowel habit for a few months. She has no other associated symptoms. She previously had laparoscopic adjustable gastric band (LAGB) insertion 8 years prior with good result (BMI pre-procedure was 56 kg/m2, and now 36 kg/m2). Her other comorbidities include hypertension and colonic diverticular disease with previous acute diverticulitis. She was organized to have an elective colonoscopy. Colonoscopy revealed tubular foreign body embedded in the wall of colon, with an entry and exit point, ~55 cm from anal verge (Fig. 1). There was also significant sigmoid and descending colon diverticular disease.
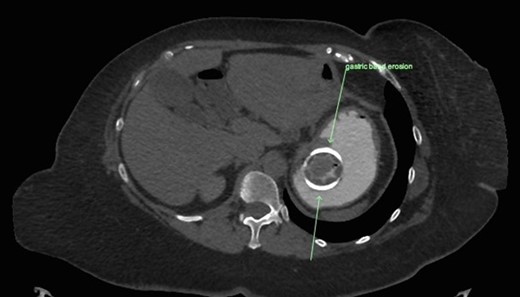
CT abdomen with oral and intravenous contrast was organized to further investigate the tubular foreign body. It revealed concurrent gastric band erosion into gastric lumen and connection tubing eroding into the posterior wall of transverse colon and exiting inferiorly (Figs 2–6). There was no evidence of any oral contrast leak from the stomach.
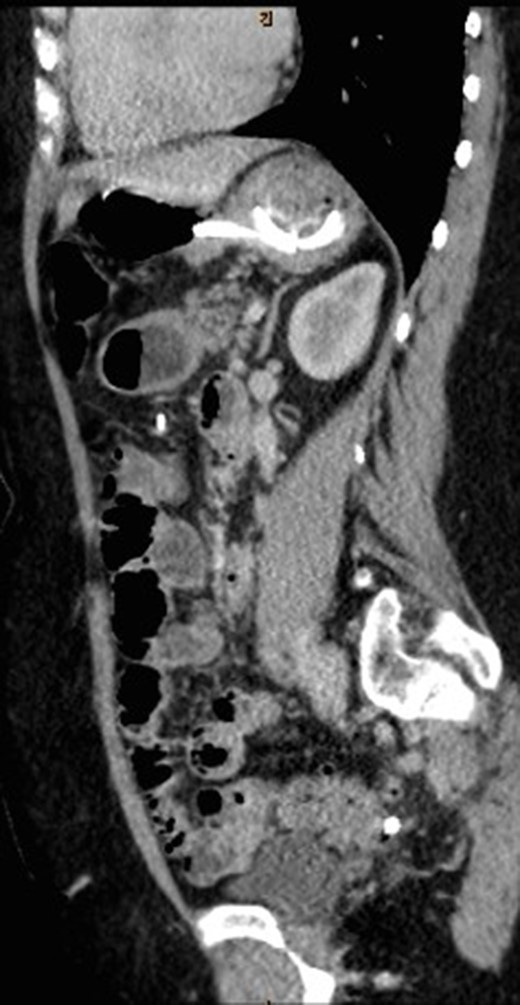
Sagittal view of CT abdomen showing the gastric band tubing eroding into posterior wall of transverse colon and exiting inferiorly.
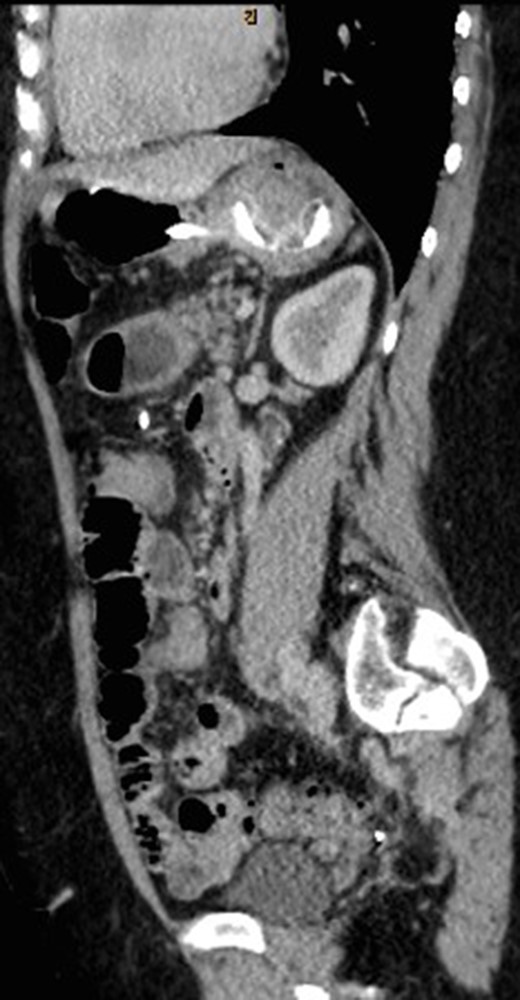
Sagittal view of CT abdomen showing the gastric band tubing eroding into posterior wall of transverse colon and exiting inferiorly.

Sagittal view of CT abdomen showing the gastric band tubing eroding into posterior wall of transverse colon and exiting inferiorly.

Sagittal view of CT abdomen showing the gastric band tubing eroding into posterior wall of transverse colon and exiting inferiorly.
This patient has previously been admitted for acute diverticulitis 4 years prior. Reviewing prior imaging did not reveal any gastric or colonic erosion. The gastric band tubing is noted to be running along the inflamed colon. Since the initial admission for acute diverticulitis, she has had multiple further acute diverticulitis episodes, which were treated with oral antibiotics. We suspect recurrent diverticulitis lead to the erosion of the gastric band into the colon and stomach.
As part of the surgical management, both colorectal and upper GI surgeon were involved in the operation. Patient underwent laparoscopic removal of gastric band and laparoscopic assisted wedge resection of transverse colon. The gastric band was removed following adhesiolysis and the gastric defect was repaired with intracorporeal suturing. The gastric band port was subsequently removed. Gastroscopy was done to ensure the repair was airtight. For the colectomy, transverse colon and splenic flexure was mobilized laparoscopically and the transverse colon was extracted through the gastric band port site for external inspection. A tract was identified passing from the antimesenteric border to colonic lumen and then along the colonic mesentery. A wedge resection performed with stapler end to side anastomosis. Flexible sigmoidoscopy was performed to confirm the anastomosis was airtight. Her post-operative recovery was uneventful, and she continued to be well on post-operative follow up in clinic. She remains well on subsequent phone follow up 12 months post operatively.
DISCUSSION
LAGB is a one of the most common bariatric procedure performed to treat morbid obesity in the past few decades. Although the number of LAGBs being inserted globally is decreasing, there is still significant number of patients with bands in situ [1]. Device related complications such as gastric erosion and connection-tubing problem are rare (1–3 and <1%, respectively) [2, 3]. It is exceedingly rare to have both complications at the same time.
Band erosion usually develops gradually over time. Several theories have been postulated as the cause of gastric band erosion. These include undetected stomach wall injury leading to chronic infectious process, chronic ischemia from band overfilling, aggressive dissection causing impaired blood supply rendering tissue susceptible to pressure ischemia [3].
There have been few case reports describing intraluminal migration of gastric band tubing, mostly associated with free end of tubing which was internalized intraperitoneally following removal of infected port [4].
Our patient is unique in that she has no predisposing factors described above.
However, she has had multiple episodes of acute colonic diverticulitis attack. We proposed that the repeated assault of intra-abdominal infection causes subacute infection of gastric tubing and gastric band. In the setting of friable colonic tissue, the tubing can then migrate intraluminal over time.
CONCLUSION
Simultaneous gastric and colonic erosion are extremely rare complication of LAGB. We propose that intra-abdominal infection increases the risk of developing erosions of gastric band and its tubing. We suggest a close follow up of all patients with gastric band who has recurrent chronic intra-abdominal infection.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST STATEMENT
Authors declare no conflict of interest.



