-
PDF
- Split View
-
Views
-
Cite
Cite
Sesi Ayodele Hotonu, Milan Gopal, Bladder injury in a child during laparoscopic surgery, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz043, https://doi.org/10.1093/jscr/rjz043
Close - Share Icon Share
Abstract
Injury to intra-abdominal organs occurs in approximately 0.2% of adult laparoscopic general surgery cases. This risk is increased in the paediatric population due to the comparatively smaller operative field. Laparoscopic appendicectomy is the most common laparoscopic procedure performed in children. Placement of a suprapubic working port is common; this is associated with a risk of bladder injury. We present our experience of managing a 6-year-old boy who sustained an extra-peritoneal bladder injury during port placement for a laparoscopic appendicectomy. We will also review the relevant current literature.
INTRODUCTION
Bladder injury is a rare recognized complication of laparoscopic surgery and is reported to occur in approximately 0.02–8.5% of adult general surgery cases [1]. The risk of bladder injury in paediatric surgery is higher than in adults due to the comparatively smaller operative space, and the tendency of the full bladder to become an abdominal organ in the infant patient.
Laparoscopic appendicectomy is one of the most common laparoscopic procedures performed in paediatric surgery [2]. Placement of ports varies between surgeons, but the most commonly used configuration involves the placement of an umbilical port, a left iliac fossa port, and a suprapubic port [3]. Bladder injury is most likely to occur in placement of the suprapubic port, especially in the presence of a full bladder. We report our experience of managing a 6-year-old boy who sustained an extra-peritoneal bladder injury secondary to port placement during laparoscopic appendicectomy.
CASE REPORT
Our patient is a 6-year-boy who was referred to our paediatric surgery tertiary centre from a district general hospital with a suspected bladder injury following a laparoscopic appendicectomy. Apart from a diagnosis of hereditary spastic paraplegia which was managed with physiotherapy, he was fit and well. He had undergone no previous abdominal surgery. His clinical history and examination at presentation suggested a diagnosis of perforated appendicitis. He had elevated inflammatory markers. A laparoscopic appendicectomy was performed using a three port technique; a 10 mm port was placed in the umbilicus using an open Hassan technique, and 5 mm ports were placed in the left lower quadrant and suprapubic region under direct vision. The bladder was emptied prior to starting the operation using an ‘in/out’ Foley catheter. The intraoperative findings were of a perforated gangrenous pelvic appendix with an associated collection. Due to this a drain was left at the end of the procedure, entering the abdominal cavity through the suprapubic port wound. He was left on intravenous broad spectrum antibiotics. Three days post operatively it was noted that a yellowish fluid was collecting around the suprapubic drain. The child was otherwise well. Biochemical analysis of the yellowish fluid revealed it to be urine. An ultrasound scan of his abdomen done by the referring hospital showed no free fluid collections. As the referring hospital lacked the facilities to further investigate a bladder injury he was transferred to our centre for further management.
At our centre, a size 6fr catheter was inserted and kept on free drainage. The suprapubic drain was removed as the urine was leaking around the tube rather than through it, and an absorbent dressing placed over the port site wound prior to further investigations. A cystogram performed via the indwelling Foley catheter showed tracking of contrast to the abdominal wall, soaking the overlying dressing (Fig. 1). There was no free intraperitoneal leak of contrast. These findings were consistent with an extra peritoneal bladder injury.
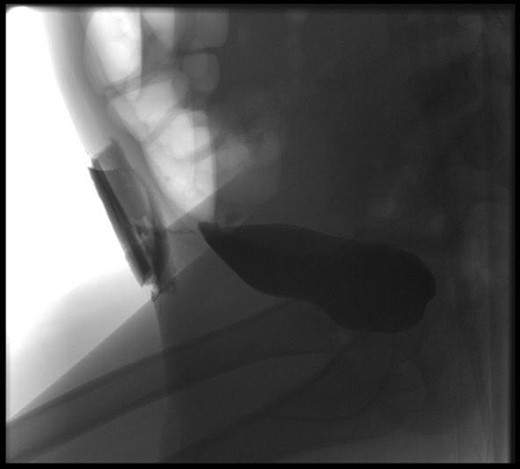
Cystogram showing tracking of contrast to the abdominal wall, and soaking the overlying dressing.
The decision was made to manage this injury conservatively. To optimize bladder drainage the urinary catheter was changed to an 8fr Foley. After 1 week, the catheter was removed. He was able to pass urine as normal, with no persisting leakage of urine through the suprapubic wound. He was kept on oral antibiotics at treatment dose for the duration of his catheterization. He had no pain or discomfort on voiding. At his 2-month follow-up appointment, the child showed no sequelae of his injury and was discharged.
DISCUSSION
Laparoscopic appendicectomy is currently one of the most commonly performed paediatric surgical procedures; its growing popularity over open appendicectomy is due to reported reduced length of hospital stay, shorter recovery time, and relative cosmesis of scars [4]. However, laparoscopic surgery is associated with a 0.2% risk of intraabdominal injury, most commonly during use of bladed or blunt trocars to insert ports [5]. Intestinal injury is the most common, followed by vascular injury [4, 5]. Bladder injury is estimated to occur in approximately 0.3–0.5% of adult laparoscopic appendicectomies [1]. This risk is increased in children due to a comparatively smaller operative field and the presence of a greater proportion of the full bladder within the abdominal cavity compared to adults. The use of a suprapubic port in laparoscopic appendicectomy is common, and is most likely to cause the bladder injury. This risk can be reduced by catherisation of the bladder prior to placement of ports [1, 5]. An ‘in/out’ technique of catheterization is often utilized safely. A cooperative child may be encouraged to void prior to induction of anaesthesia. However in the septic child requiring substantial intraoperative fluid resuscitation, the benefit of an indwelling catheter is two-fold; it allows for monitoring of resuscitation efforts, and also ensures the bladder remains empty during port placement [4]. This case demonstrates however that an empty bladder does not completely eliminate risk of bladder injury. Bladder injury in laparoscopic surgery may be intra-peritoneal or extra-peritoneal. Intraperitoneal injuries may be immediately apparent, such as when using sharp dissection inside the abdomen, or delayed such as rupture of an occult injury caused by thermal dissection of a nearby structure [5]. These usually require operative repair. Extra-peritoneal injuries, like in this case, are most commonly caused by port placement. They often present between 1 and 3 days post operatively [1]. Symptoms include urinary leakage from wound sites, lower abdominal pain and swelling, oliguria, and cystitis. A cystogram is the diagnostic investigation of choice. Other imaging modalities include ultrasound, which would demonstrate large fluid collections, and computerized tomography (CT) [1, 5]. Small extraperitoneal injuries can be managed conservatively with catheterization of the bladder for 5–7 days along with broad spectrum antibiotics. Larger injuries with associated extraperitoneal haematomas may require radiological drainage or operative exploration, washout and repair of the bladder wall if conservative measures are not effective [5].
CONCLUSION
Extraperitoneal bladder injury is a rare complication of laparoscopic appendicectomy in children. Pre-operative bladder emptying reduces the risk of this complication. Small extraperitoneal leaks may be managed conservatively with urinary catheterization and antibiotics with no sequelae. However, intra-peritoneal leakage requires operative repair.
Acknowledgements
None.
Conflict of Interest statement
None.
Funding
None.



