-
PDF
- Split View
-
Views
-
Cite
Cite
Filomena Soares, Pedro Brandão, Raquel da Inez Correia, Vítor Valente, Small bowel obstruction due to intraluminal metastasis from malignant melanoma, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz044, https://doi.org/10.1093/jscr/rjz044
Close - Share Icon Share
Abstract
The most common form of presentation of malignant melanoma is cutaneous. However, it is important to notice that it can occur in any part of the body, mostly from metastatic route. Gastrointestinal forms of symptomatic metastasis are rare, making it sometimes difficult to diagnose. We present a rare case of an 84-year-old female with a small bowel obstruction due to melanoma metastasis. She was treated with an enterectomy, with no surgical or post-operative complications. Although surgery should be reserved from symptomatic patients, some authors refer to it as a palliative treatment with improvement in long-term survival.
INTRODUCTION
Malignant melanoma accounts for 1–3% of the malignant cancers and can be found in cutaneous and noncutaneous sites. The noncutaneous presentation is relatively rare, both occurring in ocular and various mucosal sites, such as anorectal, vaginal, nasal and gastrointestinal (GI) tract [1].
The GI presentation of melanoma is most common in the small bowel, being more often a form of presentation of metastatic disease. Although some authors describe few cases of primary GI melanomas, a primary lesion in the usual sites should always be extensively searched [2].
CASE REPORT
We present the case of an 84-year-old female with a previous history of malignant melanoma of the right inferior limb, submitted to a wide excision 5 years earlier and two other surgeries of resection of in-transit metastasis.
She presented to the emergency room (ER) with clinical features of intestinal obstruction—nausea, vomiting, abdominal pain and no passing of faeces or gas in the previous 2 days. At physical examination, she was hemodynamically stable, presenting tenderness on palpation of the lower abdominal quadrants, with no signs of peritoneal irritation. Rectal examination was normal. The laboratory tests had no significant changes.
Abdominal X-ray revealed small bowel distension with multiple hydroaeric levels. Abdominal computed tomography (CT) scan (Figs 1 and 2) demonstrated distension of the small bowel due to an intraluminal mural mass with 4 cm in diameter, being the intestine collapsed distal to it. There was no evidence of other metastatic disease, including the liver.
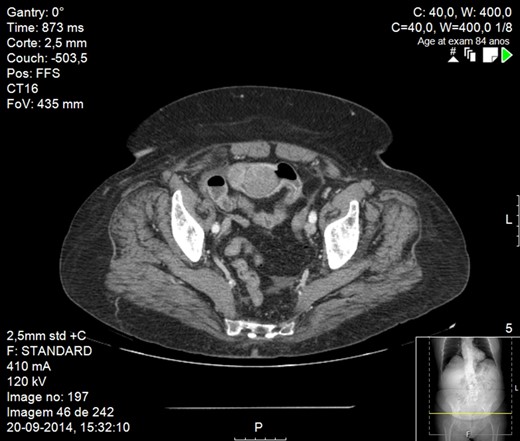
CT scan image showing small bowel obstruction due to polypoid intraluminal masses.

CT scan image showing small bowel obstruction due to polypoid intraluminal masses.
The patient underwent small bowel resection, in which we confirmed the presence of many polypoid intraluminal amelanotic masses responsible for the obstruction, located approximately 20 cm before the ileocecal valve (Fig. 3). The histological examination was consistent with metastasis of malignant melanoma with no tumoral cells on the draining lymph nodes.
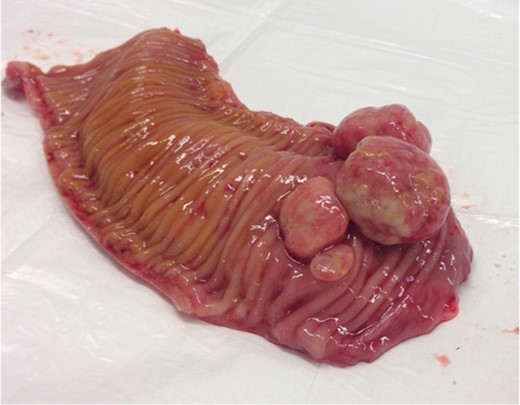
Surgical specimen: opened small bowel with several polypoid masses arising from the lumen.
The post-operative recovery was uneventful but the patient died two moths later due to disseminated disease.
DISCUSSION
Malignant melanoma is a relatively aggressive neoplasm that may metastasize virtually to any organ of the body, either by lymphatic or haematological route [3, 4]. According to post-mortem studies, gastrointestinal metastases are usually present in more than 25% of melanoma cases [5], with the most common sites being the small bowel, colon and stomach [6]. However, the clinical presentation of symptomatic GI metastases is rare.
The diagnosis should be suspected when a patient with previous history of malignant melanoma has clinical features of abdominal pain, intestinal obstruction or gastrointestinal bleeding.
The main prognostic factor in patients with stage IV disease is the site of distant metastases, with a poorer prognosis for visceral metastases (e.g. lung, liver, and gastrointestinal tract lymph node).
On this group of patients, surgery is normally reserved for symptomatic patients in need of urgent palliation (e.g. bleeding or obstructing gastrointestinal lesions), like our patient was.
Some studies suggest that resection may not only solve the symptoms but also increase long-term survival [6].
Conflict of Interest statement
None declared.



