-
PDF
- Split View
-
Views
-
Cite
Cite
Oliver William Wright, Coonoor Chandrasekar, Unusual presentation of metastatic leiomyosarcoma—right forearm swelling, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjy350, https://doi.org/10.1093/jscr/rjy350
Close - Share Icon Share
Abstract
Leiomyosarcoma (LMS) is a rare smooth muscle connective tissue tumour accounting for around 11% of soft-tissue sarcomas (Ducimetiere F, Lurkin A, Ranchere-Vince D, Decouvelaere AV, Péoc’h M, Istier L et al. Incidence of sarcoma histotypes and molecular subtypes in a prospective epidemiological study with central pathology review and molecular testing. PLoS One 2011;6:e20294). LMS are highly unpredictable tumours that can present at any site in the body, most commonly in the uterus, stomach, small intestine and retroperitoneum. There are few published case reports within the literature on the metastatic spread of LMS to skeletal muscle. We present an unusual presentation of metastatic Leiomyosarcoma in the right forearm of a 71-year-old male treated with limb-sparing surgical excision. This case report demonstrates the unusual and unpredictable nature of metastatic LMS presentation, which poses difficulty in diagnosis and management.
INTRODUCTION
Sarcomas are rare malignant mesenchymal neoplasms accounting for less than 1% of solid malignant adult tumours [1]. There are more than 70 histological types with increasing molecular subtypes arising in all anatomical sites within the body [2]. The vast heterogeneity of sarcomas therefore represents diagnostic and therapeutic challenges in clinical practice. Leiomyosarcoma (LMS) is a rare sub-type of soft-tissue sarcoma derived from smooth muscle cells accounting for 11% of all soft-tissue sarcomas [1]. While it is well researched that these tumours have a tendency to metastasise to lungs, lymph nodes, liver and bone; the occurrence of these soft tissues metastases in distal extremities has seldom been reported and reviewed within the literature. We present an interesting case report of a patient who was diagnosed and treated for metastatic LMS in the forearm.
CASE REPORT
A 71-year-old male was referred to sarcoma clinic on 11/9/2017 with a painless swelling in his right forearm. He had a previous history of primary retro-peritoneal leiomyosarcoma surgery in 2011 with subsequent liver and lung metastases for which he underwent surgical resection in January 2017. His other past medical history included benign prostatic hypertrophy (controlled with medication), otherwise he was fully mobile, fit and well. This right-hand dominant male described a gradual 3-month history of increasing painless swelling to the volar aspect of the right forearm with full function of the arm and no neurological deficit. On clinical examination, there was a soft 5 × 4 cm swelling, 5 cm proximal to wrist crease in the volar compartment of the right forearm. The swelling was fixed, non-tender with no distal neurovascular deficit and or regional lymphadenopathy. Magnetic resonance imaging (MRI) of the right forearm demonstrated a 45 × 33 × 19 mm mass in the volar aspect in close relation to the median nerve (Fig. 1). Ultrasound-guided needle core biopsy was consistent with LMS and the histology was similar to the previous LMS suggesting the possibility of metastatic LMS. Staging studies did not show any other metastatic deposits. Following multidisciplinary team discussion, he underwent planned marginal excision of the metastatic sarcoma with preservation of the median nerve. Histology confirmed LMS composed of spindle cells with eosinophilic cytoplasm with mild pleomorphism confined within the perimysium with no necrosis or vascular invasion (trojani grade 1). The patient recovered well post operatively with no neurological deficit only complicated with a mild episode of cellulitis to the wound site which fully resolved with a short course of oral antibiotics. One year after surgery, the patient has full function and use of his right hand and there is no evidence of LMS recurrence or further metastatic spread both clinically and radiologically on recent CT scan of his chest, abdomen and pelvis and MRI scan of the forearm (Fig. 2).
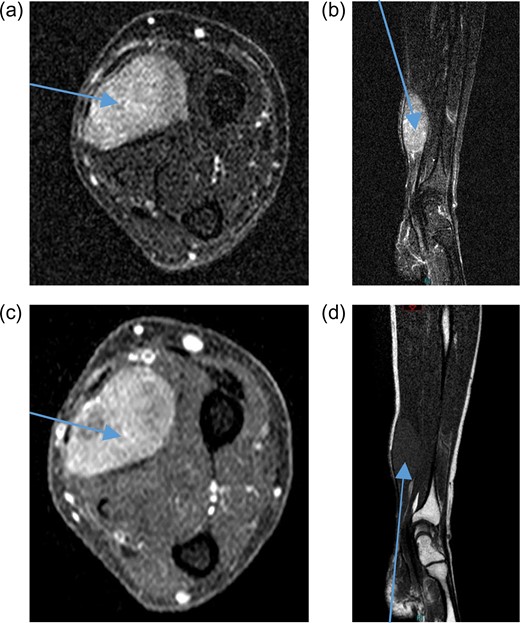
Pre-treatment contrast MRI of forearm showing large soft-tissue mas lesion involving the flexor aspect of right forearm (a) axial T2, (b) coronal T2, (c) axial T1 and (d) coronal T1.
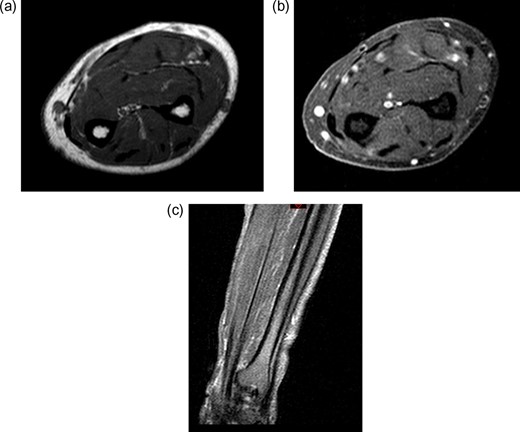
Post-treatment contrast MRI of the forearm showing curative resection and no evidence of recurrence in the flexor compartment (a) sagittal T1, (b) sagittal T2 and (c) coronal T1.
DISCUSSION
LMS is a rare type of soft-tissue sarcoma that can originate anywhere in the body, most commonly in the retroperitoneum [3]. Primary retro-peritoneal LMS are often asymptomatic and have a high propensity for haematogenous metastatic spread most commonly to the lung, thyroid, liver, brain and bone [4]. Previous research has shown that 40% of cases with primary LMS diagnosis will have co-existent distant metastasis [5]. However, while skeletal muscle metastasis has been well published in other malignancies such as bronchogenic carcinoma, breast carcinoma, melanoma and gastrointestinal tumours, there have been very few published reports of distant LMS metastasis to skeletal muscle. We have presented an unusual pattern of LMS metastasis to forearm skeletal muscle, highlighting the propensity for atypical metastatic spread of LMS.
Skeletal muscle metastasis is uncommon via haematogenous spread and therefore seldom soft-tissue masses are often associated with primary tumours or systemic malignancies such as lymphoma. Metastasis to skeletal muscle and subcutaneous tissue is very rare for LMS, with previous published data estimating an incidence of 7% for soft-tissue metastasis for LMS [6]. Very few case reports have been published demonstrating skeletal muscle metastasis from LMS. Aslan et al. [7], demonstrated a unique case of right temporalis muscle metastasis from uterine LMS in an elderly female patient. Other reported anatomical locations of LMS metastasis to skeletal muscle include: masseter, gluteus maximus, rectus abdominis, flank and thigh [4].
Soft-tissue sarcomas arising in the hand or forearm are usually small lesions detected at a relatively early stage due to the paucity of soft-tissue in this region. Despite their small size, primary sarcomas of the hand and forearm tend to be aggressive and are sometimes fatal. In addition, among LMS of all primary sites, retro-peritoneal LMS are associated with the worst prognosis with an estimated 80–87% patient mortality within 5 years [8]. Given the high degree of heterogeneity and propensity for metastatic spread for LMS, wide surgical excision is the gold standard for curative treatment. However, even when complete excision has been accomplished, local recurrence rates are high with reported figures between 40% and 77% [8]. The role of chemotherapy and radiotherapy is generally reserved for unresectable cases since reports have shown treatment to be ineffective in achieving local control and cure of disease [9]. However, some studies have shown that if surgical margins are narrow then chemotherapy and radiotherapy are beneficial [10]. Therefore, long-term follow-up with interval CT scans and clinical review at least once a year is vitally important. Consequently, soft-tissue metastatic spread of LMS can provide a significant challenge to clinicians due to the late presentation of metastatic disease in unusual locations [8]. It is therefore imperative that any atypical presentations of apparent soft-tissue masses are investigated early with a high degree of suspicion for metastatic LMS.
CONCLUSION
This case reports highlights the potential for LMS giving rise to metastatic deposits in unusual locations many years after initial presentation. Therefore, LMS patients should have long-term disease surveillance and clinicians should be vigilant for any atypical presentations for metastatic disease spread of LMS. Any unexplained soft-tissue lump will need urgent ultrasound scan and referral to a sarcoma centre, if the scans are abnormal or indeterminate.
ACKNOWLEDGEMENTS
No acknowledgements.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
There are no sources of funding or financial support.
CONSENT
Written informed consent was obtained from the patient for publication of this case report.
DISCLOSURES
The authors have no conflicts of interest or financial ties to disclose.



