-
PDF
- Split View
-
Views
-
Cite
Cite
Tariq Ali, Madison Bowles, Darius Dastouri, Neil Allen, Low thrombin tissue sealant ARTISS (Baxter), in complex primary closure after Fournier’s gangrene, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjy344, https://doi.org/10.1093/jscr/rjy344
Close - Share Icon Share
Abstract
The following case report describes the reconstruction of Fournier’s gangrene (FG) which failed initial conventional primary closure due to issues with wound edge friability, large dead spaces, and significant tension and shearing forces created by excess adipose tissue in the patient’s groin. In the first reported case that could be found in the literature ARTISS (Baxter), a low thrombin concentration fibrin sealant was used as a tissue adhesive to close the large post FG debridement wound flaps and ensure enough working time to allow for precise wound edge approximation. Employing Artiss in the closure of the large wound allowed for successful healing where simple primary closure had failed, aided an expedient recovery and reduced post reconstructive morbidity.
INTRODUCTION
Fournier’s gangrene (FG) is a subgroup of necrotizing fasciitis involving the perineal, genital or perianal regions [1] with an incidence of 1.6/100,000 males [2] Infectious organisms trigger an inflammatory response resulting in an obliterative endarteritis of surrounding vasculature [3]. This leads to vascular thrombosis of the soft tissue and ensuing necrosis [3]. The disease represents a surgical emergency and early diagnosis is imperative due to its fulminant nature, with rates of fascial necrosis noted to be as high as 2–3 cm per hour [4]. The disease mandates expeditious and radical tissue debridement which can result in extensive tissue defects requiring both morphological and aesthetic reconstruction [1].
Fibrin tissue sealants contain two major components (human fibrinogen and human thrombin) and when admixed just prior to application it replicates and augments the final stage of the coagulation cascade [5]. The resulting fibrin polymer facilitates wound healing by increasing tissue plane adherence, accelerating revascularization, minimizing inflammation, reducing haemorrhage and preventing seroma formation [6]. By virtue of their technical simplicity, fibrin sealants offer an attractive adjunct to a variety of reconstructive techniques where sutures or staples alone are expected to yield unsatisfactory results [7]. Artiss is unique in that its characteristic low concentration of thrombin (4.5IU) enables adequate time of up to 60 seconds for manipulation of tissue or flaps before polymerization and final fixation occurs [8]. In the following case report, we describe how Artiss works as a valuable tool for wound approximation during the reconstruction of FG sequelae.
CASE REPORT
A 45-year-old male, with a background of type 2 diabetes mellitus and morbid obesity (BMI 40.9) presented septic to the Emergency Department, with a one-week history of increasing scrotal pain, penile discomfort, and difficulty ambulating. He was febrile and tachycardic on presentation. Physical examination revealed a grossly swollen and oedematous scrotum with tissue necrosis evident over the right posterior hemiscrotum. Erythema and induration extended to the rectum, pubic and right inguinal regions. Biochemistry revealed a polymorphonuclear leucocytosis, hyperglycaemia and lactic acidosis. A computed tomography scan of his abdomen/pelvis confirmed a markedly oedematous right hemiscrotum with extensive subcutaneous emphysema tracking into the right inguinal region and anterior abdominal wall (Figs 1 and 2).
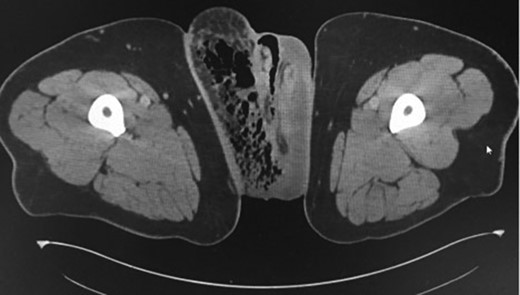
Axial CT scans of pelvic region demonstrating gas in the right groin region.
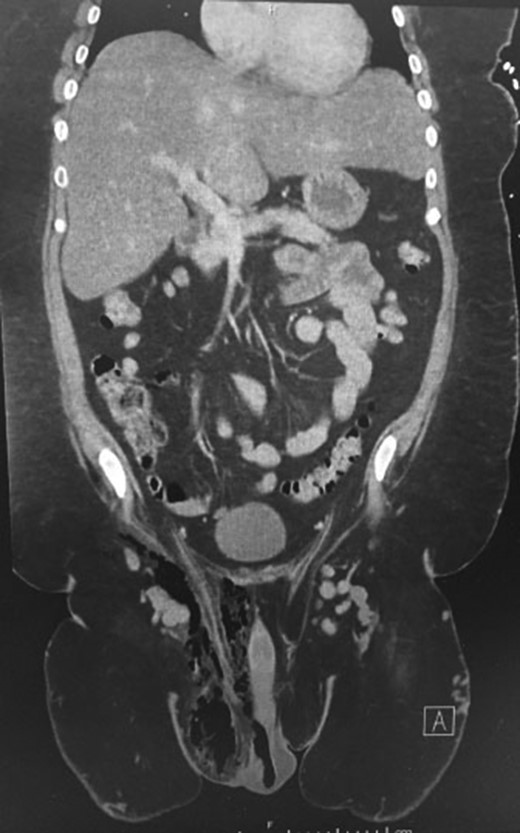
Coronal CT scans of abdominopelvic region demonstrating gas and in the right groin region.
The patient was commenced on empiric intravenous antibiotic therapy (vancomycin, lincomycin and meropenem) and was expeditiously taken to theatre by the Urology team for radical debridement of his perineum and right hemiscrotum. Intraoperatively, necrosis of the scrotum and perineum extended over the inguinal ligament towards the right ASIS and the pathognomonic ‘dishwater fluid’ of liquefied necrotic tissue was seen. The right hemiscrotum required complete dissection and sparing of the penis, testicles, and rectum was achieved (Fig. 3).

Over the following two weeks the patient returned to theatre for four further washouts (Day 2, Day 5, Day 9 and Day 12).
Vacuum assisted closure (VAC) therapy was employed in the interim. Given the patient’s habitus, employing negative pressure dressings posed significant challenges; exudate from the wound, the adverse contours of the region and the forces generated by the patient mobilizing all contributed to loss of dressing seal. Further difficulties arose when the patient refused a faecal diversion system resulting in frequent faecal contamination of the perineal aspect of the wound.
The patient was referred to the Plastic Surgery team for delayed primary closure. He was commenced on maximal dose Loperamide and a pressure mattress was requested for his convalescence. On Day 19, the wound was thoroughly washed and delayed primary closure was attempted by approximating the wound edges using simple subcutaneous horizontal mattress sutures with 2-0 Monocryl. Unfortunately wound dehiscence was evident by Day 24.

On Day 25 the patient was taken back to theatre for another attempt at closure. The wound edges were freshened up, and 2-0 Vicryl was used as a untied half-buried mattress (Barron's) sutures along the length of the wound. 4 ml of Artiss was atomized using surgical air to allow a thin and even covering of the wound cavity. The wound was then approximated and held in place for 90 seconds. The sutures were then hand-tied, and non-adhesive dressings were applied (Fig. 4).
Follow-up at 1 month revealed complete closure of the wound with minimal de-epithelialization of the medial flap. No significant post-operative wound complications occurred and no further intervention was required (Fig. 5).

DISCUSSION
Following FG debridement, reconstruction of tissue defects is required to achieve satisfactory functional and cosmetic result [3]. The best results are achieved by primary closure, however tension free closure is only possible with the smallest of defects in normal habitus patients [9]. For larger defects or those under tension, several reconstructive techniques exist including skin grafts, scrotal musculocutaneus flaps, fasciocutaneous flaps, transposition of the testes into a subcutaneous pocket in the upper thigh and pedicled myocutaneous flaps [9].
In this case, the defect was suitable for primary closure, however the need to avoid potential hollow viscus injury precluded the use of adequate deep sutures, and the shearing forces created by excess fatty tissue in the groyne proved too great for closure with subcutaneous sutures alone. Proximity to the anus predisposed the wound to significant risk of infection and consequent wound dehiscence. The rotational forces placed on the area during ambulation necessitated a reconstructive method that provided significant tensile strength.
Artiss acted as an adjunct to wound edge closure by working as a deep tissue adhesive. This reduced the dead space and therefore the forces generated by local movements. The low thrombin component of Artiss (as compared to other tissue sealants) allowed for greater working time to accurately close the wound.
In similar cases, where the anatomical region and patient factors preclude the use of other techniques, Artiss serves as a valuable and successful means of achieving accurate and full surface tissue approximation whilst also reducing the possibility of complications including haematoma or seroma [7, 9, 10]. .
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
Summary of Product characteristics for ARTISS, frozen. 1.3 Product information. Version 06f_Sep11. 1-18



