-
PDF
- Split View
-
Views
-
Cite
Cite
Jonathan P Rehfuss, Jeffrey E Friedman, Sanda A Tan, Lawrence L Lottenberg, Lindsey E Goldstein, Cecal volvulus caused by internal herniation after roux-en-y gastric bypass surgery, Journal of Surgical Case Reports, Volume 2018, Issue 9, September 2018, rjy241, https://doi.org/10.1093/jscr/rjy241
Close - Share Icon Share
Abstract
Cecal volvulus is the rotation of a mobile cecum resulting in a large bowel obstruction. We present the case of a 55-year-old female who underwent a roux-en-y gastric bypass in 2003 and presented to the emergency department with worsening abdominal pain, distention and obstipation. Roentgenogram demonstrated a 14 cm colon suggestive of sigmoid volvulus, but CT scan showed rectal contrast abruptly ending in the distal transverse colon, mesenteric swirling and a distended cecum, consistent with cecal, rather than sigmoid, volvulus. Upon surgical exploration the majority of the small bowel, cecum and ascending colon had herniated through the transverse mesocolon defect created during her prior gastric bypass. The bowel was reduced through the mesenteric defect, and an ileocecectomy was performed. This is, to our knowledge, the first reported case of cecal volvulus caused by an internal hernia through a mesocolon defect created during a prior roux-en-y gastric bypass operation.
INTRODUCTION
Cecal volvulus is the rotation of a mobile cecum, typically in a meso-axial or organo-axial fashion, resulting in a large bowel obstruction. Predisposing anatomic characteristics include incomplete intestinal rotation during embryogenesis and insufficient retroperitoneal attachments of the right colon, either congenitally or as a result of mobilization during a prior operation. Adhesions from previous surgery, distal colonic obstruction and colonic atony are also risk factors for cecal volvulus. We present a very unusual case of cecal volvulus resulting from herniation of the cecum, ascending colon and a substantial portion of small bowel through a large transverse mesocolon defect created during a roux-en-y gastric bypass operation 13 years earlier.
CASE REPORT
A 55-year-old female with a medical history remarkable for hypertension, chronic pain and cigarette smoking was admitted to the hospital after presenting to the emergency department with several days of worsening abdominal pain, distention and obstipation. She had been evaluated multiple times in prior months for similar symptoms and treated aggressively for constipation. Her surgical history included an open roux-en-y gastric bypass in 2003 resulting in a 140 pound weight loss and an exploratory laparotomy for a perforated gastric ulcer in 2005. Upon admission, she was hemodynamically stable without a leukocytosis. Physical exam revealed left-sided abdominal distention and moderate tenderness. Roentgenogram demonstrated a markedly dilated 14 cm loop of colon in the left upper quadrant concerning for a sigmoid volvulus (Fig. 1A). Subsequent computed tomography (CT) scan showed rectal contrast extending into the transverse colon, mesenteric swirling and a distended cecum, consistent with cecal, rather than sigmoid, volvulus (Fig. 1B and C).
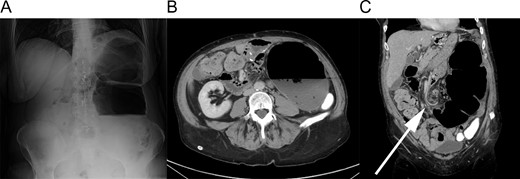
Radiographic findings. (A) Upright plain film showing massive colonic distention. (B) Axial slice of CT scan showing a 14 cm diameter colon. Note the oral contrast filling the descending colon. (C) Coronal slice of CT scan. The arrow indicates mesenteric swirling in the mid-abdomen.
On emergent exploratory laparotomy we found that the majority of the small bowel, dilated cecum and proximal ascending colon had herniated through the large transverse mesocolon defect created during her roux-en-y gastric bypass. The bowel, all of which was viable, was reduced through the mesenteric defect and into the correct anatomical position. An ileocecectomy with a handsewn ileocolonic anastomosis was performed given the extensive serosal injury from the acutely dilated cecum. To prevent future herniation, the large mesenteric defect was closed around the roux limb. The patient recovered quickly and was discharged home on post-operative Day 4.
DISCUSSION
While cecal volvulus is generally a result of an overly mobile cecum twisting on itself, the literature does contains reports of it being caused by a variety of unusual causes including endometriosis, Meckel’s diverticulum, herniation through the Foramen of Winslow and incarceration within a giant ventral hernia. However, ours appears to be the first reported case of cecal volvulus caused by an internal hernia (IH) through a mesocolon defect created during a prior roux-en-y gastric bypass operation. The unusual nature of this complication contributed to her delay in diagnosis.
Roux-en-y gastric bypass is among the most commonly performed bariatric operations in the USA. In the late post-operative period, IH, a feared complication, occurs with a reported incidence of 1–11% [1]. Three anatomical sites for internal herniation exist following a retrocolic approach: between the roux limb mesentery and the transverse mesocolon (Petersen’s space), directly through the transverse mesocolon defect or in the mesenteric opening behind the biliary limb. Efforts to reduce the likelihood of developing an IH include passing the roux limb antecolic rather than retrocolic, obliterating potential hernia sites with suture and, more recently, closing defects with a stapler device. Despite studies comparing these different techniques, no consensus exists on the operative conduct which most greatly minimizes the risk of post-operative IH. A meta-analysis, published in 2015, concluded that antecolic configurations are generally associated with lower rates of IH compared with retrocolic positioning. While direct closure of defects would seem to reduce the risk of IH, empiric evidence suggests that it may have no effect, or even increase the rate of IH [2]. This may be a result of the defect not remaining closed or opening only partially into a smaller defect large enough to incarcerate bowel but too small to allow spontaneous reduction [3].
Interestingly, a retrospective analysis of over 900 laparoscopic gastric bypass operations at a single institution identified an association between the speed at which excess weight is shed during the first post-operative year and the occurrence of IH. Patients who developed an IH were 1.8 times more likely to have experienced periods of extremely rapid weight loss (defined as a rate of excess weight loss in the top decile) compared with those who did not have an IH [4]. The mechanism underlying this association is unknown, but one hypothesis is that the rapid loss of mesenteric fat does not permit sufficient time for potential hernia site closure. Patients in this analysis were followed for only 2 years, and the mean presentation of IH was 15.6 months post-operation. Only 14% of the patients received a retrocolic reconstruction and only 9% of IH involved the colon mesentery.
Our patient was predisposed to cecal volvulus because of an excessively mobile cecum, which was congenital since her right colon had never been surgically mobilized. Her retrocolic roux-ex-y configuration likely increased her risk of IH. Whether any or all of her defects were closed during her gastric bypass operation in 2003 is unknown, and the effect that this might have had is unclear based on the existing body of literature. It seems unlikely that her degree of excess weight loss during the first post-operative year would have had any influence on her development of IH 13 years later.
The surgeon must have a high index of suspicion for IH in any patient with a history of gastric bypass presenting with a clinical picture suggestive of bowel obstruction. If internal herniation has occurred, the contents are likely to be small bowel, yet colonic incarceration is possible. Large bowel obstruction caused by IH likely requires surgical treatment; certainly in the case of associated cecal volvulus, either an ileocecectomy or right hemi-colectomy is indicated to relieve the immediate problem and prevent recurrence. No data currently exist to guide the decision to close (or not) the internal defect to prevent a second episode of IH.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- abdominal pain
- computed tomography
- dilatation, pathologic
- emergency service, hospital
- gastric bypass
- hernias
- intestine, small
- intestines
- mesentery
- mesocolon
- surgical procedures, operative
- cecum
- colon
- cecal volvulus
- sigmoid volvulus
- large intestinal obstruction
- obstipation
- gastric bypass, roux-en-y
- ascending colon
- transverse colon
- transverse mesocolon
- exploratory surgery



