-
PDF
- Split View
-
Views
-
Cite
Cite
Joseph Rassam, Andrew E Healey, Sarah J Wood, Harriet Jane Corbett, A challenging abdomino-scrotal hydrocele—successful resolution with the help of interventional radiology guided sclerosis, Journal of Surgical Case Reports, Volume 2018, Issue 9, September 2018, rjy232, https://doi.org/10.1093/jscr/rjy232
Close - Share Icon Share
Abstract
Abdomino-scrotal hydrocele is a rare condition that presents in male infants. There is no consensus in the literature over treatment. We present the case of a 4-year-old boy with what was thought to be a straight forward congenital hydrocele that persisted despite ligation of a patent processus vaginalis and a Jaboulay procedure. A subsequent Magnetic Resonance Imaging scan identified a large intra-abdominal component connecting to the scrotum. Laparoscopic excision of the intra-abdominal component was performed successfully, but the hydrocele persisted. The hydrocele resolved without complication following two episodes of image intensifier guided sclerotherapy carried out by the interventional radiology team.
INTRODUCTION
A hydrocele is a collection of serous fluid within the tunica vaginalis or alongside the spermatic cord. Hydroceles are common in male infants and are nearly always ‘communicating’ hydroceles due to patency of the processus vaginalis (PPV) [1]. Non-communicating hydroceles, typically found in adults, occur when the processus vaginialis is closed but the tunica vaginalis produces a surplus of fluid [1]. Communicating hydroceles in young children usually resolve spontaneously therefore surgical intervention is not typically considered until the child is at least 2–3 years of age [2]. An exception may be when there is additional intraperitoneal fluid, for example, in the presence of a ventriculoperitoneal shunt or peritoneal dialysis.
CASE REPORT
A 4-year-old boy presented to clinic with a 7-week history of scrotal swelling. Examination demonstrated a right-sided hydrocele with no extension up the spermatic cord. Ligation of a right-sided PPV was performed; the procedure was straightforward but the PPV within the inguinal canal had a loculated distal component.
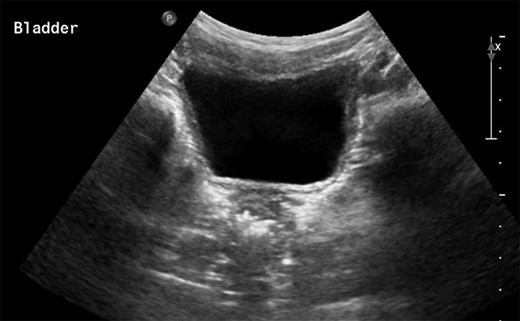
The patient presented 2 weeks post-operatively with enlargement of the scrotal hydrocele. A non-communicating encysted component was suspected. A watchful waiting approach was planned but the swelling grew further so a Jaboulay procedure was performed. After postoperative swelling had resolved it was clear that the scrotal hydrocele persisted. After 2 months an ultrasound scan (USS) was performed and was largely insignificant other than the identification of the scrotal hydrocele itself (Fig. 1).
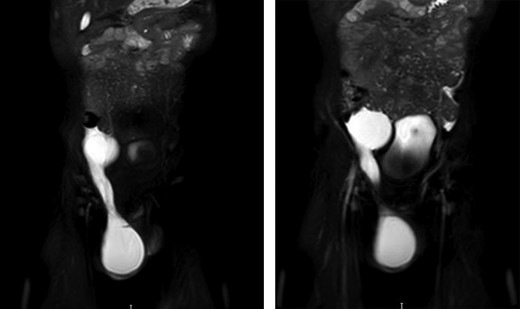
Persistence of the hydrocele and a differential diagnosis of lymphatic malformation were discussed by a multidisciplinary team and an MRI scan was advised. This displayed a large fluid filled structure adjacent to the bladder which was not present when the USS was conducted. The structure tracked down the inguinal canal to the right-sided scrotal hydrocele (Fig. 2).
The patient underwent laparoscopy, prior to which USS showed that the scrotal element was empty, but the intra-abdominal component was present. Surgery identified a single simple cyst adjacent to the right side of the bladder and communicating with the inguinal component. The cyst was excised diligently to preserve the vas and vessels. Histology confirmed a simple cyst.
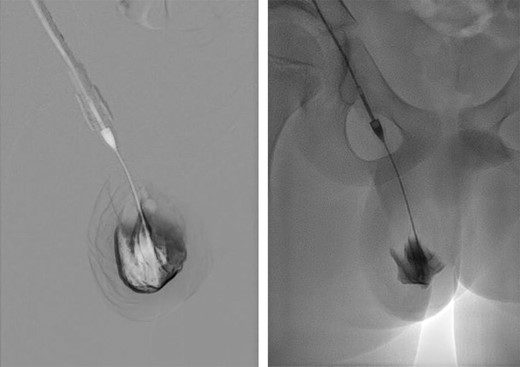
Six weeks post-operatively the hydrocele persisted. Time was allowed for the hydrocele to resolve but during the following 3 months the hydrocele continued to enlarge and cause discomfort. The case was discussed with the interventional radiology team and treatment by aspiration and sclerosis (Fig. 3) was offered, for both the scrotal sac and a residual intra-abdominal component, if present. At the time of treatment, the lesion was shown to be confined to the scrotum. Following two treatments with sodium tetradecyl sulphate foam, 2 months apart, resolution was confirmed on both clinical and USS examination. The testes were normal upon final USS 3 months after completion of sclerotherapy.
DISCUSSION
Hydroceles in children commonly resolve following PPV ligation. In this case, the persistence of the hydrocele following PPV ligation was assumed to be due to secretion of fluid within the loculated distal component. Thus, a Jaboulay procedure was performed which failed to resolve the hydrocele and in hindsight may have been unnecessary. Following this an intra-abdominal component was considered, but the initial USS failed to reveal it, suggesting that there was no fluid within that component at that time. A subsequent MRI scan revealed the intra-abdominal component and proved the value of repeated imaging in atypical cases. Excision of the intra-abdominal component alone was insufficient to resolve the hydrocele which was then successfully managed by sclerotherapy, supporting the hypothesis of a secretory distal component.
Abdomino-scrotal hydroceles are rare, with a reported incidence of <3% in boys [3–5]. They are frequently diagnosed with USS and may be suspected if examination of the groin is atypical. The aetiology of abdomino-scrotal hydrocele is not well defined. One hypothesis is that sustained enlargement of a scrotal hydrocele extends along the inguinal canal and into the extra-peritoneal space [6]. There is no consensus regarding management of abdomino-scrotal hydroceles. Some authors advise operative management in all, whilst others support non-operative management since spontaneous resolution is well described [7, 8]. It should be noted that surgery, be it via the inguinal, laparoscopic or scrotal approach, is associated with a complication rate that can be as high as 80% [7, 9].
The relatively late and acute onset of the hydrocele made this case unusual. Furthermore, the fluctuating nature of the intra-abdominal component made the diagnosis elusive initially; a lymphatic malformation was also considered. Laparoscopic excision of the intra-abdominal cyst was undertaken, the logic being that this was the primary source of fluid. Following successful excision of the cyst, the scrotal pseudo sac was now considered the sole source of the fluid. It was hoped that with time the lesion would resolve but increasing size and symptoms led to consideration of further intervention. One option was to repeat a Jaboulay-type procedure but neither the family nor surgical team were keen on this due to an uncertain chance of resolution and a high chance of testicular damage and, thus, sclerotherapy was considered.
Sclerotherapy is an interventional radiological procedure regularly used to treat cystic lesions and lymphatic malformations, particularly when they are not amenable to surgical resection. Recent literature suggests that sclerotherapy has a place in the treatment of hydroceles in the adult population [8, 10]. However, there is little literature relating to children. The suggested mechanism of action is that the sclerosant acts as an irritant, eroding the epithelium of the sac, destroying its ability to produce fluid. Repeated treatments are often required but their minimally invasive nature makes this acceptable to most patients. Complications are typically minor and self-limiting. In this case, the extremely low chance of testicular and spermatic cord damage, was a key factor.
CONCLUSION
Abdomino-scrotal hydrocele should be considered in children with atypical groin examination, recurrent or persistent hydroceles. USS is usually the best mode of diagnostic imaging; repeated imaging is advised in atypical cases. Sclerotherapy of the scrotal component was curative and should be considered at the early stage of management of abdomino-scrotal hydroceles, potentially avoiding traditional surgery.
CONFLICT OF INTEREST STATEMENT
None declared.



