-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel Lim, Raymond Kostin, The rare and unusual presentation of a gastric perforation in the setting of a large diaphragmatic hernia: a case report and literature review, Journal of Surgical Case Reports, Volume 2018, Issue 9, September 2018, rjy238, https://doi.org/10.1093/jscr/rjy238
Close - Share Icon Share
Abstract
Diaphragmatic hernias are either congenital or acquired defects in the diaphragm that permit passing of abdominal contents into the chest cavity. Individuals with large diaphragmatic hernias associated with a gastric perforation have rarely been reported in literature and can have serious mortality rates. Herein, we present a case of gastric perforation in the setting of a significant sized diaphragmatic hernia. The value of the current report compared to previously published cases is the sub-acute nature and lack of any indicative features on initial presentation which can lead to misdiagnosis and serious morbidity later in life.
INTRODUCTION
A diaphragmatic hernia is a defect or opening in the diaphragm that allows bulging of abdominal contents into the thoracic cavity. Congenital diaphragmatic hernias are the most common type, while spontaneous diaphragmatic hernias are less frequently detected [1]. Despite being rarely reported, perforation and incarceration of the diaphragmatic herniation are disturbing and may lead to significant morbidity and even death [2]. Moreover, the diagnosis is challenging and the condition may get worse with delayed diagnosis [3]. Our report sheds light on management of a gastric perforation in the setting of a large diaphragmatic hernia in a clinically stable patient. Our findings are consistent with only one other published report [4], and further investigations are warranted for a better outcome.
CASE PRESENTATION
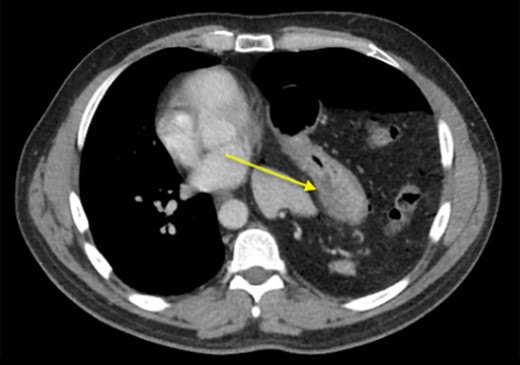
We present a 44-year-old male patient came to the emergency department complaining of right upper quadrant abdominal pain. The patient reported taking over-the-counter (OTC) ibuprofen intermittently for a past few months due to backaches. His past medical history is only positive for falling off a 15 feet ladder at the age of 15 years old. Upon examination, he had right upper quadrant abdominal tenderness, a heart rate of 90 beats/min and a respiratory rate of 20 breaths/min on room air. The patient clinical status was stable and looked well. Chest x-ray showed a moderate left hemidiaphragm elevation with bowel contents overlying the left chest (Fig. 1). Of note, a large amount of air inferior to the right hemidiaphragm was indicative for pneumoperitoneum. Laboratory investigations were immediately carried out and revealed a white blood cell count (WBC) of 4.5 × 109/L (normal range: 4–11 × 109/L). The WBC remained at the normal level until the end of the patient’s admission. Further imaging studies were ordered due to the peculiar coexistence of x-ray findings and stable clinical status. The computed tomography (CT) scan showed a contracted left lung with severe volume loss and just mild aeration of the left upper lung (Fig. 2). No definite left pneumothorax was seen. The majority of the left hemithorax was filled with abdominal contents including the stomach, spleen, pancreatic tail, left kidney, splenic flexure of the colon, and small bowel loops. A small hypodense focus was observed within the intra-thoracic stomach and extended to the stomach wall, with mild adjacent stranding of fat and a small amount of free fluid. We suspected the presence of perforated gastric ulcer secondary to non-steroidal anti-inflammatory drugs (NSAIDs) usage. The upper gastrointestinal (GI) series was performed and did not show any extravasation, indicating that there was some other source or the gastric perforation had walled off. The patient was thus managed conservatively; his diet was advanced and the patient discharged home on Day 4.
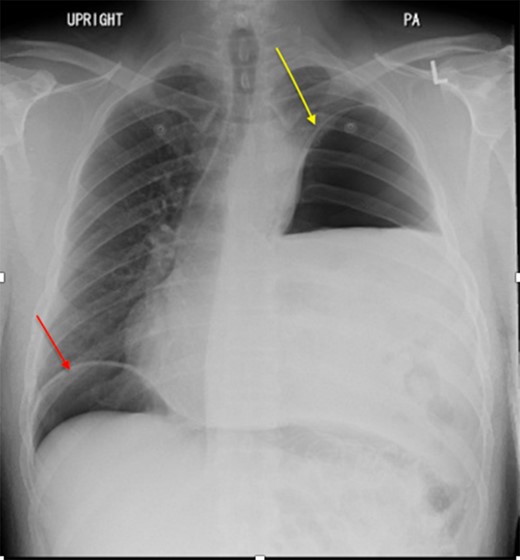
Chest x-ray showed a moderate left hemidiaphragm elevation with bowel contents overlying the left chest.

CT scan showing collapse of left lung and left diaphragmatic hernia.
Two days later, the patient re-presented to the emergency department with left-sided pleuritic chest pain. The heart rate was 92 beats/min and the respiratory rate was 23 breaths/min on room air. The patient was stable, looked well, and his pain resolved almost entirely at time of examination. Clinically relevant labs showed a WBC of 8 × 109/L (normal range: 4–11 × 109/L). The CT did not show any significant enlargement of pneumoperitoneum; however, significant rightward shift of the mediastinum was noted. So we suggested worsening tension in the left hemithorax with further collapse of the left lung (Fig. 3). Despite being clinically stable, the mediastinal shift which was not present on the previous admission was concerning and thus the patient was taken to the operating room with the decision to repair the hernia. A left thoracotomy was used to enter the chest cavity. There was severe atelectasis of upper and lower lobes. We immediately noted a large hernia sac which encompassed the entire chest cavity and the remaining diaphragmatic muscle was significantly thinned out. The hernia sac was opened in order to identify the source of the pneumoperitoneum seen on imaging which we had suspected to be of gastric origin. Upon examination of the abdominal contents which required meticulous dissection off the herniated diaphragm from chronic adhesions, we were able to identify a well-developed perforated gastric ulcer on the anterior surface of the greater curvature of the stomach (Fig. 4). This ulcer was resected with a wedge GIA stapler and the hernia was subsequently closed by bringing the muscles together and imbricating the closure with the redundant sac using prolene sutures. Upon closure, we did not place a mesh due to the possible contamination from the gastric perforation. When the repair was complete and the patient taken off the one-lung ventilation, his lungs immediately pinked up and re-expanded. Overall, the patient tolerated the procedure very well without any post-operative complication. Two days later, we carried out an upper GI series which showed no evidence of any extravasation and his diet was advanced. On the sixth post-operative day, the patient was discharged home. He was re-evaluated in clinic 2 weeks later and continued to progress well with a stable repeat chest x-ray (Fig. 5).
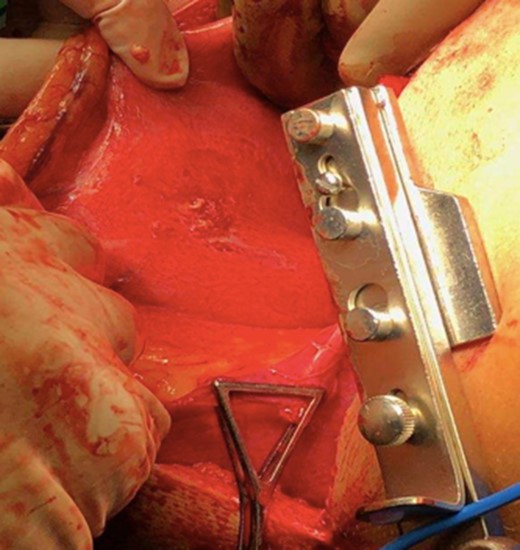
Intra operative photo depicting gastric perforation on greater curvature.

Chest x-ray on follow-up visit post-operative showing stability of repair.
DISCUSSION
In this report, we present a case of an adult male with a well-developed perforation on the anterior surface of the greater curvature of the stomach in the setting of diaphragmatic hernia. The highlight of this case report is the sub-acute presentation observed in our patient despite having this serious exacerbation of diaphragmatic herniation and a gastric perforation. The right upper quadrant abdominal pain he initially presented with was mild and his abdominal exam was benign. The location of the pain was another oddity which initially led to the workup for cholecystitis by the ED department but can later be explained on CT by the free air trapped between in the liver and the diaphragm. If it was not for the abnormal chest x-ray and subsequent CT scan after the workup for cholecystitis was negative, this patient would have been misdiagnosed and his hospital course may have resulted in a worse outcome. It is noteworthy mentioning that previous reports stated that the delayed diagnosis of gastric perforation of diaphragmatic hernia can increase morbidity and mortality [3].
Either congenital or acquired diaphragmatic hernias are usually diagnosed through the integration of radiograph, CT scan and contrast swallow. The congenital type is the most common form and it occurs originally because of diaphragmatic defect during embryological development. Most of the congenital types can be diagnosed during the neonatal or perinatal period. However, some of them may be diagnosed in adulthood if missed during the said period [5]. The location of our patient’s diaphragmatic herniation was not consistent with a late-presenting congenital diaphragmatic hernia being that the postero-lateral and anterior parts of the diaphragm are considered the most commonly detected locations of congenital diaphragmatic hernia [6]. Our patient’s diaphragmatic herniation was located in the center of the left hemidiaphragm.
Although adults may have diaphragmatic hernias that were not diagnosed at an early age, trauma is the most common cause of adult-onset diaphragmatic hernias. Although it has been ~30 years since our patient fell off a ladder and has been relatively asymptomatic, we cannot exclude this trauma as the inciting cause. The gastric perforation of adult-onset diaphragmatic hernia together with stable clinical status was previously reported by Vinnicombe et al. [4]. Nevertheless, their patient had neither recent nor past history of trauma.
Although perforations or incarcerations that take place in the setting of diaphragmatic hernias are rare. Once detected, prompt diagnosis and proper management are essential given the associated morbidity and mortality are considerably high [7].
Much of the delayed diagnosis can be attributed to the non-specific presentation of some of these patients as in our case as he originally presented with mild right upper quadrant abdominal pain. This is a unique case of an individual with a sub-acute presentation associated with a gastric perforation in a setting of a large diaphragmatic hernia with the lack of serious symptoms, which is consistent with the previous report from Vinnicombe et al. [4]. These are the only two known case reports in literature to report two disease entities occurring simultaneously that can both be associated with high morbidity and mortality if left untreated. Fortunately for both patients, the stable clinical status of the patient allowed for the well planned out surgical approach resulting in good outcomes in both scenarios.
CONFLICT OF INTEREST STATEMENT
None declared.



