-
PDF
- Split View
-
Views
-
Cite
Cite
Usman Waheed, Crystal-Jade Haughton, Athena Tudino, Katie Carson, Emma Mancini, Bifid omental band: an unusual cause of small bowel obstruction, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy210, https://doi.org/10.1093/jscr/rjy210
Close - Share Icon Share
Abstract
Small bowel obstruction (SBO) in adults is most commonly caused by postoperative adhesions, hernias or neoplasms. Here, we report a unique case of SBO caused by a bifid omental band in a 65-year-old female who presented with abdominal pain, nausea and vomiting. Abdominal and pelvic computed tomography showed dilation of mid-small bowel suggestive of partial SBO. An abdominal x-ray and small bowel series confirmed a high grade SBO. When initial conservative treatment failed, exploratory laparoscopy was performed and it was discovered that the patient had a bifid omental band encircling the small bowel, resulting in obstruction. Following resection of the band, she had an uneventful post-surgical recovery.
INTRODUCTION
Small bowel obstruction (SBO) is the significant mechanical impairment or complete arrest of the passage of contents through the small intestines. Symptoms may include acute onset of cramping pain, obstipation, abdominal distension, nausea and vomiting. More than 65% of all SBOs in developed countries result from intra-abdominal adhesions, followed by less common etiologies such as hernias, Crohn disease, neoplasms and other miscellaneous causes [1, 2]. Symptoms include nausea and vomiting, constipation and/or obstipation, cramping abdominal pain and abdominal distension [2]. A high level of clinical suspicion is needed to diagnose the condition, and prevent the possible progression from obstruction to ischemia and perforation. Plain radiographs are often the first imaging studies obtained upon suspicion of SBO, followed by computed tomography (CT) of the abdomen which has a sensitivity of over 95% in detecting obstruction [1, 2]. Most cases of uncomplicated SBO can be treated conservatively with fluid resuscitation and nasogastric suction for decompression, whereas surgical management is often required where there is evidence of complete obstruction, bowel ischemia or perforation [1, 2]. While the common causes of SBO are well-represented in the literature, rarer etiologies including SBO caused by a band of greater omentum without a history of laparotomy are not reported. Here, we report a rare case of SBO caused by an omental band in a 65-year-old African American female with no prior history of laparotomy or inflammatory bowel disease.
CASE REPORT
A 65-year-old African-American female presented to the Emergency Department complaining of diffuse, crampy abdominal pain and non-bilious vomiting that started earlier in the day following a meal. She reported one semi-solid bowel movement in the past 24 h which did not provide any relief of symptoms. Review of systems was otherwise negative and vitals were normal. The patient reported a surgical history consisting of no intra-abdominal surgery. On physical examination, the abdomen was soft and non-distended with no guarding or rigidity noted. Hyperactive bowel sounds were present in all four quadrants, with bilateral lower quadrant tenderness to palpation.
Laboratory studies were remarkable for leukocytosis, and an elevated lactate that improved with hydration (Fig. 1), while urinalysis was unremarkable. Abdominal CT scan obtained at this time demonstrated a partial SBO in the mid-small bowel as well as inflammation and thickening of the duodenum. A small bowel series was ordered, and showed high grade SBO (Figs 2–5).
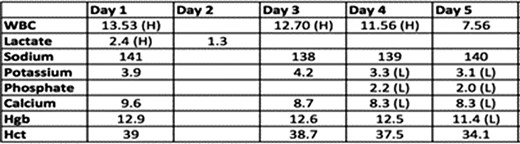
Lab results on Day 1 of admission through to Day 5 of hospital stay, notable for elevated lactate and leukocytosis on admission. (H) Indicates a value that is above the reference range, while (L) indicates a value below the reference range.

Fluoroscopic barium study demonstrating oral contrast agent progression through the small bowel at 5 min after ingestion.

Fluoroscopic barium study demonstrating oral contrast agent progression through the small bowel at 30 min after ingestion.
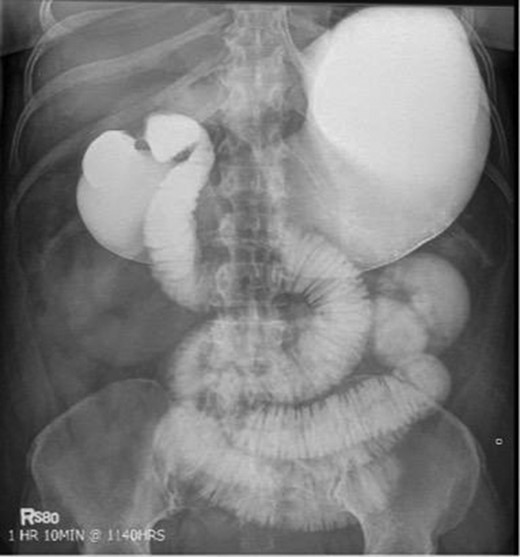
Fluoroscopic barium study demonstrating oral contrast agent progression through the small bowel at 1 h after ingestion. The stomach is distended, with dilated bowel loops throughout the abdomen.
Laparoscopy showed an obstruction of the small bowel caused by a bifid omentum that wrapped around the distal jejunum, adhering to its walls (Fig. 6). A clear transition point was appreciated. The band of omentum was lysed and the proximal bowel decompressed. The patient remained in hospital and had an uncomplicated postoperative recovery.

Fluoroscopic barium study demonstrating oral contrast agent progression through the small bowel at 5 h after ingestion. Dilated bowel loops can be visualized throughout the abdomen, and transit time is delayed. Impression—high-grade distal small bowel obstruction.
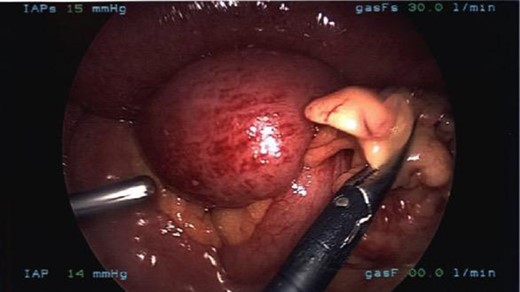
Laparoscopic visualization of the transition point of the obstruction in the distal jejunum caused by a band of omentum.
DISCUSSION
The omentum is a highly vascularized sheet of fibrous and adipose tissue that supports the intestines and abdominal organs [3]. It functions in neovascularization, clearance of bacteria and foreign material from the peritoneal cavity, supplies leukocytes and enables migration of neutrophils, and adheres to areas of contamination. The etiology of omental band formation includes congenital development, postoperative formation and from inflammation [3]. This patient’s lack of prior abdominal surgery, except for C-section, makes a congenital etiology more likely.
On review of literature, SBO caused by omental banding is very rare with only few reported cases in the literature [4–7]. Sinwar reported a case of a 42-year-old male with SBO secondary to greater omental encasement without previous history of abdominal surgery. Biopsy ultimately demonstrated tubercular granuloma on histological exam causing chronic inflammation [4]. The second case involved a 31-year-old male with SBO secondary to lesser omental encasement and only mild inflammation of the omentum on histological exam, also without any prior history of abdominal surgery [5]. A third case involved a 47-year-old woman with SBO secondary to greater omental banding with a history of chronic constipation [6]. In this case, biopsy of the omental band showed fat necrosis on histological exam [6]. Literature review also revealed one report of a bifid omentum that had undergone torsion, causing acute abdominal pain [7]. We believe this is the fourth reported case of SBO caused by omental banding and the first reported case of SBO caused by a bifid omentum band.
It must be considered whether the history of previous cesarean section could have lead to the SBO. While possible, it is unlikely that the omental banding discovered was related to her C-section, as the obstruction was found proximal to the site of the previous incision and did not involve the abdominal walls. The overall incidence of SBO following gynecological procedures is ~11% and only 0.1% after cesarean section [8, 9].
This unique case of SBO caused by a bifid omental band demonstrates the need for a high level of clinical suspicion for SBO even in patients without prior history of abdominal surgery, and identifies omental banding as an etiology that must be considered separately from adhesions.
CONFLICT OF INTEREST STATEMENT
None declared.



