-
PDF
- Split View
-
Views
-
Cite
Cite
Veronika Kröpfl, Benedikt Treml, Stefan Scheidl, Monika Lanthaler, Michael Nogler, Ingo Lorenz, Barbara Friesenecker, Dietmar Fries, Gerhard Pierer, Dietmar Öfner-Velano, Necrotizing fasciitis of the lower extremity caused by perforated sigmoid diverticulitis—a case report, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy198, https://doi.org/10.1093/jscr/rjy198
Close - Share Icon Share
Abstract
Diverticulosis of the sigmoid colon is a common condition and occurs more often in elderly patients. A well-known complication is infection or even perforation which often requires surgery. Necrotizing fasciitis as a complication of perforated diverticulitis is very rare. Here, we present a case of a covered perforated diverticulitis in an immunosuppressed patient leading to life-threatening necrotizing fasciitis requiring extracorporeal membrane oxygenation. Either hematogenous or local dissemination via the inguinal canal seemed the most probable mechanism of leg infection leading to hip articulation.
INTRODUCTION
Colonic diverticulosis is a common disease in the western world [1]. It can appear in every part of the intestine, with over 95% occurrence in the sigmoid colon. As patient age increases its incidence does correspondingly. Diverticula may occur because of a decreased resistance of the intestinal wall, a changed pressure gradient between the intestinal lumen and the abdominal cavity or even low fiber diet. The typical complications of colonic diverticulosis are diverticulitis, bleeding or perforation [1]. A perforated bowel can cause severe infections like sepsis or peritonitis, in case of a covered perforation a retroperitoneal abscess results.
Necrotizing fasciitis is a rare but severe infection of any layers of the soft tissue with high mortality rates due to sepsis [2, 3]. The classic pathogen is Streptococcus pyogenes, however, infections with multiple bacteria (streptococci, aerobic microorganisms an anaerobic microorganisms) may occur as well [2, 3]. The fundamental treatment is radical debridement of the infected tissue. Necrotizing fasciitis as a result of a perforated sigmoid diverticulitis is barely described in the literature [4, 5].
We present a patient with necrotizing fasciitis of the left leg caused by a perforated diverticulitis of the sigmoid. Interestingly, here the resulting abscess spread more down to the left lower extremity as into the abdominal cavity. The most probable infection route to the lower extremity were dissemination of bowel germs via the inguinal canal or via blood stream infection.
CASE REPORT
A 49-year-old woman required urgent osteosynthesis of a periprothetic femur fracture after trauma to the left hip. Due to long standing (~48 y) rheumatoid arthritis the patient was immunosuppressed with corticosteroids and adalimumab and had underwent multiple joint replacements since her childhood. At the third postoperative day after osteosynthesis of the fractured femur she suffered from large bilateral pulmonary embolism at the orthopedic patient-department. Two days later septic shock had developed, apparently from a necrotizing fasciitis of the leg. The perioperative antibiotic treatment with clindamycin was extended empirically with cefeprime and fosfomycine. A whole-body scan was performed which revealed free gas in the retroperitoneum as a sign of a covered perforated diverticulitis (Fig. 1). Due to increased systemic infection signs (CRP, elevated WBC, PTC) and life-threatening patient's condition a multidisciplinary decision was made to first treat the necrotizing fasciitis. Immediate debridement of the necrotic tissue, including the subcutaneous tissue to the fascia of the leg, was performed by plastic surgeons (Fig. 2). Postoperatively multiple organ dysfunction developed, including acute lung failure, the patient required veno-venous extracorporeal membrane oxygenation (vvECMO).
As anticoagulation was required for vvECMO surgical treatment of the abdominal focus was excluded. A CT-guided drainage of the intra-abdominal abscess was performed after stabilization the patient within 2 days, the drained fluid revealed pus. Interestingly, microbiological testing of the soft tissue debridement showed Enterococcus faecium and Escherichia coli being the causative pathogens of the necrotizing fasciitis.
After stabilization and ECMO removal, the patient had to undergo hemicolectomy with an ileostomy due to a now perforated caecum at the 20th postoperative day. Several days later using a negative pressure therapy system abdominal closure was performed.
During the following postoperative days infect parameters decreased and the patient was extubated.
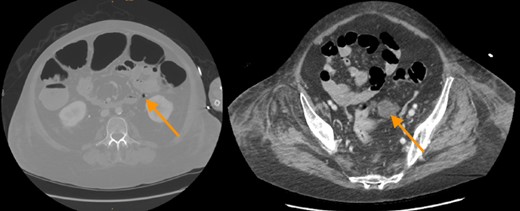
CT-scan revealed free gas and fluid in the retroperitoneum as a sign of a covered perforation of colonic diverticula.

Preoperative status of the left leg; right: picture shows the left leg immediately after radical debridement.
More than 7 weeks later on the ICU an infection of the osteosynthesis was suspected due to increasing infection signs and lack of an abdominal focus. Several functions and revisions of the retention around the hip and the osteosynthesis were performed. Despite a continuous antifungal therapy since the 14th postoperative day (using first fluconazole and later echinocandines) microbiological testing revealed infection with Candida albicans. Because of resistance to antifungal therapy, several bouts of sepsis and massive impaired healing due to immunosuppression over decades, disarticulation of the lower extremity was performed by orthopedic surgeons after 2-month ICU stay. Thereafter the patient stabilized slowly and was discharged from ICU a month later. After another 2 months and a total of 5 months in hospital the patient was discharged finally back home.
DISCUSSION
Perforation of colonic diverticulosis mostly requires urgent surgery. Necrotizing fasciitis as a very scarce complication of perforated colonic diverticulitis always needs aggressive surgical therapy [4, 6]. Two our knowledge there are only three reports of necrotizing fasciitis caused by perforated colonic diverticulitis. Two of them describe necrotizing fasciitis of the thigh or leg. In one of these cases amputation of the leg was performed [4], in the other cases urgent laparotomy and Hartmann's procedure were reported [5]. In our case, the patient experienced a necrotizing fasciitis due to a covered colonic perforation. With a large pulmonary embolism, fulminant septic shock, vvECMO, in our opinion debridement of the necrotic tissue was the first choice. Due to nearly 4 decades of immunosuppression in rheumatoid arthritis late onset of abdominal symptoms could have occurred as well. Anti-TNF therapy can cause serious infections due to reduced patient's immunity [7]. In summary, the patient survived three potential life-threatening conditions: large pulmonary embolism, fulminant septic shock and an infected femur osteosynthesis, which is owed to an excellent collaboration of a multidisciplinary team of intensivists, anesthesiologists, general, plastic and orthopedic surgeons, radiologists and microbiologists. Nevertheless, physicians should be alert to signs and symptoms in immunosuppressed patients.
CONFLICT OF INTEREST STATEMENT
The authors whose names are listed immediately below certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest.
FUNDING
The authors declare no financial or any other type of support.



