-
PDF
- Split View
-
Views
-
Cite
Cite
Bojana Misheva, Roy Hajjar, Frédéric Mercier, Frank Schwenter, Herawaty Sebajang, Conservative management of pelvic sepsis with severe shock and multiple organ dysfunction syndrome after rubber-band ligation of internal haemorrhoids: surgery is not the only option, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy199, https://doi.org/10.1093/jscr/rjy199
Close - Share Icon Share
Abstract
Rubber-band ligation (RBL) is a safe and cost-effective approach to internal haemorrhoids. Potential side effects include pain, bleeding, urinary retention and occasionally pelvic sepsis and systemic inflammatory response syndrome (SIRS). At-risk patients are mainly those with immunocompromising conditions. Although aggressive surgical debridement or diverting colostomy appear to be obvious options when patients’ life is threatened, their superiority to conservative measures has not been proven. We present the case of a 58-year-old female patient who presented 48 h after a RBL with pelvic pain, dysuria and leukocytosis. Her condition deteriorated rapidly that ventilator and inotropic support were required for a severe SIRS for almost 10 days. Laparoscopic exploration and imaging showed a rectosigmoiditis, ascites and superficial rectal necrosis with no transmural damage requiring an emergent surgery. Conservative management could possibly be a valid option in post-RBL pelvic sepsis even when severe associated multiple organ failure is present.
INTRODUCTION
Rubber-band ligation (RBL) has been introduced as a treatment for internal haemorrhoids a few decades ago by Blaisdell and Barron, and was used since with little to no side effects [1, 2]. RBL is established as a cost-effective and efficient treatment for first- to third-degree internal haemorrhoids. It works by inducing fibrosis, retraction and fixation of the haemorrhoidal cushions [3]. Although it is a safe procedure, some common complications exist, such as pain, bleeding, thrombosis, prolapse and urinary retention.
Pelvic sepsis is a rare but serious complication of this procedure. The latter usually develops 48 h after the operation and generates dysuria, perineal pain, fever and sometimes systemic sepsis. Several cases of pelvic sepsis were formally detailed in the literature after RBL, and many of them were fatal [4]. The mainstay of treatment is not clearly defined as conservative and surgical approaches both yielded favourable results. Active surgical debridement seems to be a more logical approach in severely ill patients. However, data on its superiority to conservative management are lacking.
CASE PRESENTATION
A 58-year-old female patient is diagnosed with internal haemorrhoids and undergoes RBL. Her past medical history includes osteoporosis, dyslipidemia and depression. Forty-eight hours after the procedure, she presented back to the emergency room for pelvic pain and dysuria. Physical examination did not reveal any necrosis or signs of infection. Management of her symptoms consisted of empirical intravenous antibiotics, ciprofloxacin and metronidazole, and clinical observation.
Her condition did not improve and her white blood count (WBC) increased significantly (24 000/μL). She was consequently transferred to a referral centre where she was brought to the operating room for an exploration of the surgical site. The band was removed and a small superficial abscess was drained. A computed tomography (CT) scan of the abdomen and pelvis showed a rectosigmoiditis with a moderate to severe amount of ascites. No pneumatosis was noted. An exploratory laparoscopy was thus performed to rule out rectal necrosis, and revealed an important amount of serous ascites. The patient was suffering after the surgical procedure from a severe systemic inflammatory response syndrome (SIRS) and required several days of intensive care. Due to clinical deterioration and persistent leukocytosis (25 000/μL), she was transferred to our tertiary care centre with a suspicion of ischaemic colitis.
Upon arrival, her hemodynamic and respiratory status deteriorated rapidly and ventilator support was necessary for an acute respiratory distress syndrome (ARDS). The antibiotics’ spectrum was broadened to a carbapenem. A colonoscopy to the mid-transverse colon was performed and showed a superficially necrotic 2 cm segment in the lower rectum with petechial mucosa.
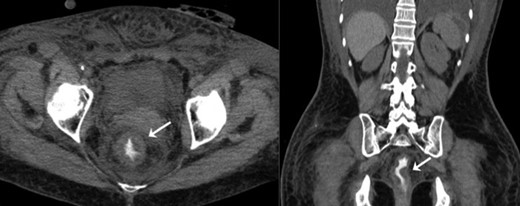
After 72 h of inotropic support with vasopressors, aggressive volemic resuscitation, ventilator support and antibiotics, a modest improvement was noted. WBC count decreased slightly from 30 000 to 23 000/μL. A repeat abdominopelvic CT scan was performed four days after the transfer and revealed once again the presence of a circumferential thickening of the rectosigmoid colon without pneumatosis (Fig. 1). The state of shock subsided gradually and the patient was extubated after a total of 9 days of ventilator support. She was transferred to the floor before being discharged from the hospital a few days later. She recovered progressively from the intensive care unit myopathy and the prolonged intubation, and benefited afterward from intensive rehabilitation.
At follow-up appointments, the patient was clinically better, but still complained of muscular weakness and poor exercise tolerance up to several months after the episode.
Three years after the events, a colonoscopy was performed and was normal. The patient was followed by a respirologist for persistent but improving dyspnea that was deemed secondary to severe deconditioning during the hospital stay. No evidence of a residual cardiorespiratory injury was objectified.
DISCUSSION
We hereby present the case of a 58-year-old woman with post-RBL severe pelvic sepsis, and associated shock and multiple organ failure (MOF), which was successfully treated conservatively.
Pelvic sepsis is an extremely rare complication of internal haemorrhoids RBL. A review of 39 studies including 8060 patients undergoing RBL revealed post-banding complications in 14% of them, including pain (5.8%), haemorrhage (1.7%), anal fissure or fistula (0.4%), and infection (0.05%) [5, 6].
As expected, severe perineal or abdominal pain, urinary retention, fever and leukocytosis could be features of perineal sepsis. In previous reports, some patients attended the emergency room more than once with these symptoms before pelvic sepsis was diagnosed [4]. Clinical presentation could therefore be sometimes misleading and a severe underlying complication is not always easy to suspect in patients undergoing this procedure. The scarcity of this adverse event makes the identification of its most specific and sensitive symptoms complex.
From what we experienced in our case, the support measures were the mainstay of the treatment since the capillary leak syndrome was the main issue to address. In the literature, patients who developed severe septic complications and organ failure were for some human immunodeficiency virus positive or had an objectified infectious lesion such as a cellulitis or gangrene [7–9]. Interestingly, despite the excessive systemic response, our patient did not show any signs of transmural tissue necrosis requiring aggressive surgical debridement. Hence, the role of the surgeon in such a case is to evaluate if a surgery will benefit the patient or not. A defunctioning colostomy or a perineal tissue debridement would have probably not added much to the maximal conservative medical treatment, and possibly complicated further the hospital stay.
Surgical intervention in a severely ill patient with a postoperative complication may sometimes be reasonable. This case shows that conservative management could be a valid approach as surgical intervention with a diverting stoma or an ischiorectal exploration might not necessarily be more efficient. Early recognition of this complication could probably prevent significant deterioration and hasten rapid referral to specialized care. Reports on such morbid cases are lacking, and early manoeuvres to slow the inflammatory response are yet to be elucidated.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- ascites
- systemic inflammatory response syndrome
- hemorrhage
- debridement
- cost effectiveness
- dysuria
- laparoscopy
- leukocytosis
- ligation
- necrosis
- pain
- pelvic pain
- shock
- surgical procedures, operative
- urinary retention
- ventilators, mechanical
- colostomy procedure
- diagnostic imaging
- rubber
- multiple organ dysfunction syndrome
- hemorrhoids, internal
- sepsis, pelvic
- transmural
- conservative treatment
- emergency surgical procedure
- inotropic support



