-
PDF
- Split View
-
Views
-
Cite
Cite
Srinivas Bojanapu, Anand Nagar, Siddharth Mehrotra, Vivek Mangla, Shailendra Lalwani, Amitabh Yadav, Naimish Mehta, Samiran Nundy, Penoscrotal swelling—an unusual occurrence in a patient with an anastomotic leak following ileostomy closure, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy197, https://doi.org/10.1093/jscr/rjy197
Close - Share Icon Share
Abstract
Diverting loop ileostomy is a frequently done procedure accompanying colorectal surgeries. Dreaded complication is anastomotic leak. Early identification of anastomotic leak and apt management is required for better outcomes. Most often leak presents with fever, abdominal pain, rigidity, fever and hemodynamic instability. We report a rare occurrence of penoscrotal oedema in a patient with anastomotic leak and spontaneously subsiding with drainage of leaked contents.
INTRODUCTION
Ileostomy closures are among the most common operations performed in surgical practice, and are associated with an anastomotic leak rate ranging from 0 to 3% [1]. These leaks usually present with abdominal pain, fever and features of peritonism. We describe a case in which a patient presented with penoscrotal oedema and abdominal distension. These features resolved after percutaneous drainage of the intra-peritoneal collection.
CASE REPORT
This 50-year-old male had, 4 months previously, undergone an anterior resection of a recto-sigmoid adenocarcinoma, non-anatomical resection of a liver metastasis and diverting loop ileostomy. The pathological report was a moderately differentiated adenocarcinoma and he subsequently received seven cycles of adjuvant chemotherapy. Two weeks after the last chemotherapy cycle he had a contrast study through the distal limb of his ileostomy which was normal. He then underwent a side-to-side hand sewn ileo-ileal anastomotic closure and started passing flatus and stools from the third postoperative day (POD). On POD 4 however he developed lower abdominal distension and a plain X-ray of the abdomen revealed air to be present in the colon and rectum with a few prominent small bowel loops. He then developed massive painless penoscrotal swelling, On local examination the genitals were not tender and there was no elevation of the local temperature (penoscrotal oedema image, Fig. 1). Blood investigations revealed a haemoglobin level of 12.8 g/dl, total leucocyte count of 5900/mm3, serum creatinine of 0.85 mg/dl, total protein 5.18 g/dl and albumin 2.95 g/dl. A urologist’s opinion was sought who opined that the patient might be having common iliac vein thrombosis but a Doppler study of the lower limb and pelvic veins was normal. However the abdominal distension persisted although he was passing flatus and stools. CECT of the abdomen was done on POD-6 and this revealed a large irregular air containing collection extending from the right subhepatic region along the paracolic gutter into the pelvis as well as a fluid collection in the lesser sac extending along the greater curvature of the stomach (CT images). Three percutaneous drains were then inserted—one each in the subhepatic region, pelvis and the left lesser sac and 1500 ml of faeculent content was removed. The patient was kept nil by mouth, started on parenteral nutrition and his antibiotics were upgraded. Over the next 3 days the effluent decreased and the fluid became serous. The penoscrotal oedema also subsided after 4 days (Figs 2–5). On POD-12, a CT scan of the abdomen with oral contrast was done again (CT images), which showed a decreased size of the collection and no well-defined area of extravasation or leak of contrast outside the bowel lumen. The drains were then removed, he was started on oral liquids and later put on a soft diet and discharged on POD-20.

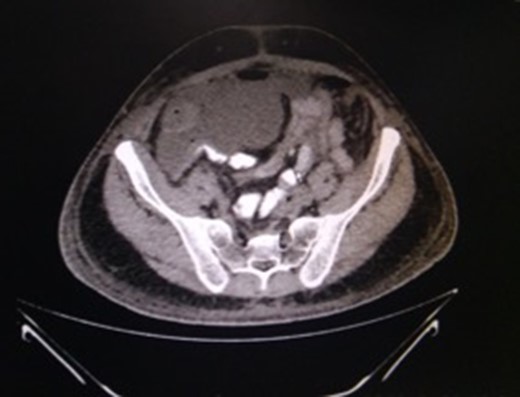
CT-abdomen showing pelvic collection. Source: Department of Radiology, Sir Ganga Ram Hospital, New Delhi.
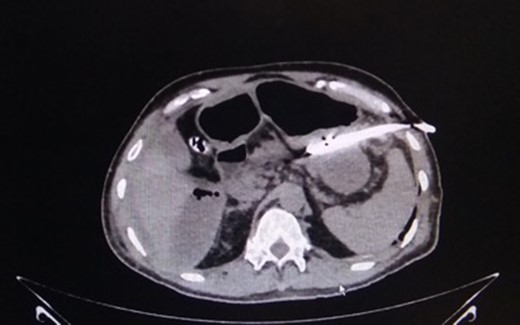
CT-image of drain in situ draining intra-peritoneal leak contents. Source: Department of Radiology, Sir Ganga Ram Hospital, New Delhi.

Penoscrotal oedema subsided after draining intra-abdominal collection. Source: Department of Surgical Gastroenterology and Liver Transplantation, Sir Ganga Ram hospital, New Delhi.

Follow up at 60 days. Source: Department of Surgical gastroenterology and Liver Transplantation, Sir Ganga Ram Hospital, New Delhi.
DISCUSSION
Anastomotic disruption is a dreaded adverse outcome after ileostomy closures and presents with abdominal pain, fever, abdominal rigidity, tachycardia and is often associated with haemodynamic instability. In these cases, urgent return to the operating room for peritoneal washout and faecal diversion is sometimes required and prolonged stays in the intensive care unit and death are not uncommon. The mortality rate for such an anastomotic leak from a ileostomy in the literature is ~2–3% [2].
Some patients ultimately found to have an anastomotic leak develop a more insidious presentation, often with low-grade fever, prolonged ileus or failure to thrive [3].
We report a case of ileostomy closure developing penoscrotal oedema followed by abdominal pain, distension, fever and tachycardia. This may have occurred because the leaked bowel contents entered the scrotal sac through a narrow but patent processus vaginalis (the patient did not have an inguinal hernia). However, an extensive Internet search done using the terms penoscrotal oedema, stoma closure and intestinal anastomosis did not reveal any case report of penoscrotal oedema as a complication after stoma closure. We report what we consider to be the first such observation of a patient who had undergone ileostomy closure and post-operatively developed penoscrotal oedema which subsided when the peritoneal fluid was drained while the anastomotic leak healed spontaneously.
CONFLICT OF INTEREST STATEMENT
None declared.



