-
PDF
- Split View
-
Views
-
Cite
Cite
F Sertic, T K Rajab, A Ali, Surgical management of iatrogenic left main coronary artery dissection, Journal of Surgical Case Reports, Volume 2018, Issue 6, June 2018, rjy121, https://doi.org/10.1093/jscr/rjy121
Close - Share Icon Share
Abstract
This is the case of a 40-year-old female diagnosed with NSTEMI. She underwent coronary angiography and suffered from type F left main coronary artery dissection. After hemodynamic stabilization, she was transferred to the nearest cardiothoracic surgery unit and underwent emergency coronary artery bypass graft (CABG) surgery. This report highlights important concepts in the management of a rare complication and emphasizes the surgical treatment decision-making, underlying an unusual but effective treatment approach.
INTRODUCTION
Iatrogenic left main coronary artery (LMCA) dissection is a rare complication of coronary angiography and percutaneous coronary intervention. Its incidence has been reported to be around 0.07% [1, 2]. The clinical presentation of coronary artery dissection is extremely variable: the spectrum can vary from a completely asymptomatic patient to severe hemodynamic instability leading to cardiac arrest. This is closely related to the severity of the dissection based on the National Heart Lung and Blood Institute classification.
Type A represents minor radiolucent areas within the coronary lumen during contrast injection with little or no persistence of contrast after the dye has cleared. Type B are parallel tracts or a double lumen separated by a radiolucent area during contrast injection, with minimal or no persistence after dye clearance.
Type C appears as contrast outside the coronary lumen with the persistence of contrast after dye has cleared from the lumen. Type D represents spiral luminal filling defects, frequently with excessive contrast staining of the dissected false lumen. Type E appears as new, persistent filling defects within the coronary lumen. Type F represents those that lead to the total occlusion of the coronary lumen without distal antegrade flow. Types A and B are usually benign, whereas types C–E should be considered potential emergencies. Based on the presentation, the available treatment options include conservative management, bail-out stenting and coronary artery bypass graft surgery.
This report describes the surgical management of a patient who suffered iatrogenic LMCA dissection during coronary angiography. The aim of the report is describe important concepts in the management of the patient and emphasize the treatment decision-making.
CASE REPORT
A 40-year-old female was admitted to her local hospital with a history of atypical chest pain at rest and a Troponin level of 60 ng/l. Therefore, she was diagnosed with an NSTEMI. Her risk factors for cardiovascular disease were hypertension and smoking. Her past medical history included left internal carotid artery dissection 5 years previously, which had been complicated by a stroke.
She was loaded with aspirin and ticagrelol and she underwent diagnostic angiogram on day 4 post hospital admission.
At the beginning of the procedure, the left main stem was engaged, however dampened pressure was noted and a test shot showed left main stem occlusion with dissection (Fig. 1).
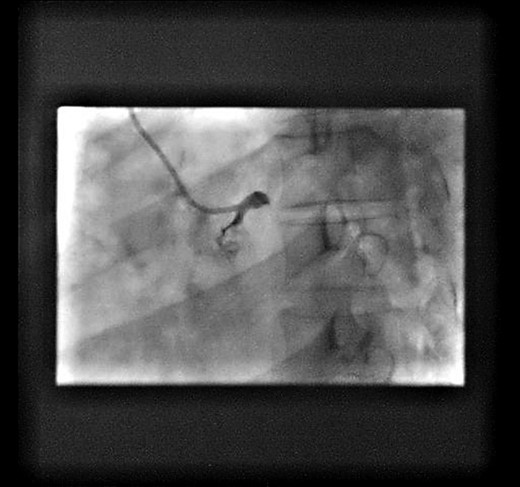
Test shot showing left-main-stem occlusion with dissection (National-Heart-Lung and Blood-Institute class F).
The patient acutely became hemodynamically unstable and suffered a cardiac arrest. Cardiopulmonary resuscitation was started and the patient was intubated. Return of spontaneous circulation (ROSC) was achieved with inotropes, vasopressors and intra-aortic balloon counterpulsation. Following ROSC, angiographic wires were passed into the coronaries. However, the operator was unable to wire the true lumen of the circumflex artery (Fig. 2).
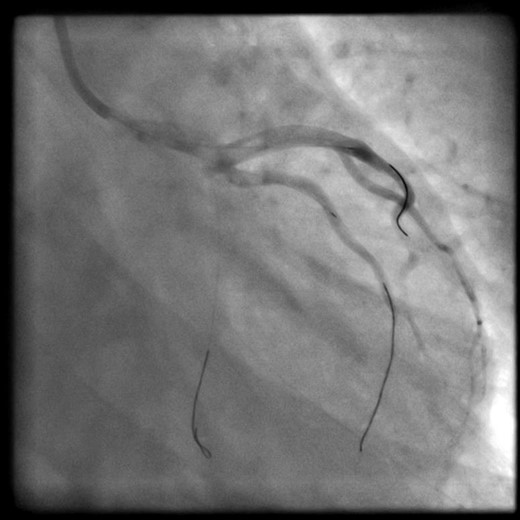
Wires left into the coronaries during transfer. LAD and intermediate: true lumen successfully wired. Cx: unable to wire true lumen.
At this point, decision was made to transfer the patient to our cardiothoracic unit for emergency coronary artery bypass graft. The patient was transferred to our unit with the angiographic wires left on purpose into the coronaries.
After arrival to our cardiothoracic unit, the patient was immediately taken to the operating room. Transoesaphageal echocardiography demonstrated a poor-left-ventricular-function (ejection fraction 29%) with anterior, antero-septal and antero-lateral regional wall motion abnormalities. Sternotomy was performed and cardiopulmonary bypass established with mild hypothermia (34 C°). Antegrade cardioplegia was administered and asystole was achieved. On visual inspection, the coronaries appeared extensively dissected therefore the arteriotomies were elongated proximally and distally until the true lumen could be identified. Subsequently two saphenous vein grafts were grafted onto the LAD and OM1, respectively. In order to identify the true lumen, the arteriotomy was extended past the dissection point in case of the OM1 and guided by the wire in case of the LAD. Proximal anastomoses were constructed on cross-clamp to avoid coronary malperfusion from changes in the hemodynamics affecting the dissection flaps. Following completion of the anastomosis, the wires were removed from the coronaries. The patient was then successfully separated from the cardiopulmonary bypass with inotropic (IABP, Dopamine and Adrenaline) and vasopressor (Noradrenaline and Vasopressin) support. The IABP was removed on post op Day 4 and all the inotropes and vasopressors were weaned off by post-operative Day 7.
She made an uncomplicated further recovery and was discharged home on post-operative-Day 12. On 6 months follow-up, she is well and making good progress with good daily activity.
DISCUSSION
Coronary artery dissection is twice as likely to occur during percutaneous coronary intervention when compared to diagnostic coronary angiography [1]. The risk factors accounting for this feared complication include unusual coronary anatomy or location, small coronary ostia, operator experience, presence of coronary atherosclerosis, older age, hypertension, connective tissue disorders, aortic root calcification and diabetes. Furthermore, certain types of angiographic catheters and wires (e.g. pressure wires) have been associated with increased risk of dissection (Judkins, Amplatzer, EBU, Q-curve, Castillo and Sones) as well as vigorous hand-injection of contrast medium, subintimal passage of the guide-wire or inappropriate handling of the guide-wire catheter has been associated with coronary artery dissection [3, 4].
This kind of emergency is one of the few exceptions to LIMA-to-LAD grafting. The surgeon should not waste valuable time harvesting the LIMA when there is active myocardial ischemia.
This case report highlights several important points. First, patients can be stabilized by leaving angiographic guidewires in the true lumen of the dissected artery in order to allow blood flow to the myocardium by preventing the complete obliteration of the true lumen. Second, the guidewires will help the surgeon in the operating room to distinguish between the true and the false lumen of the dissected arteries. Last, in the era of interventional cardiology emergency coronary artery bypass graft surgery still have an essential role in the management of complex coronary artery dissection.
Conflict of Interest statement
None declared.



